Executive Summary
Spaceflight is associated with many factors which may promote kidney stone formation, urinary retention, and/or Urinary Tract Infection (UTI). According to the International Space Station (ISS) mission predictions supplied by NASA’s Integrated Medical Model, kidney stone is the second most likely reason for emergency medical evacuation from the ISS, with sepsis (urosepsis as primary driver) being the third. Alterations in hydration state (relative dehydration), spaceflight-induced changes in urine biochemistry (urine supersaturation), microgravity-induced alterations in fluid dynamics and position of abdominal structures, and changes in bone metabolism (increased calcium excretion) during exposure to microgravity may all contribute to the increased risk of urinary health issues. This medical technical brief describes the conditions of urinary retention, UTIs, and renal stones, and how they are affected by spaceflight conditions as well as outcomes and countermeasures used to prevent them.
Relevant NASA-STD-3001 Technical Requirements
Volume One
- [V1 3001] Selection and Recertification
- [V1 3002] Pre-Mission Preventive Health Care
- [V1 3003] In-Mission Preventive Health Care
- [V1 3004] In-Mission Medical Care
- [V1 3007] Medical Evacuation
- [V1 3008] In-Mission Evacuation to Definitive Medical Care
- [V1 3016] Post-Mission Health Care
- [V1 3018] Post-Mission Long-Term Monitoring
- [V1 4019] Pre-Mission Nutritional Status
- [V1 4020] In-Mission Nutrient Intake
- [V1 4022] Post Mission Nutritional Assessment and Treatment
- [V1 4027] In-Mission Bone Countermeasures
Volume Two
- [V2 6004] Nominal Vehicle/Habitat CO2 Levels
- [V2 6026] Potable Water Quality
- [V2 6109] Water Quantity
- [V2 7001] Food Quality
- [V2 7022] Body Waste Management Privacy
- [V2 7023] Body Waste Management Provision
- [V2 7024] Body Waste Accommodation
- [V2 7035] Urine per Crewmember
- [V2 7038] Physiological Countermeasures Capability
- [V2 7043] Medical Capability
- [V2 7100] Food Nutrient Composition
- [V2 7102] Body Waste Quantities
- [V2 11013] Suited Body Waste Management
- [V2 11014] LEA Suit Urine Collection
- [V2 11028] EVA Suit Urine Collection
- [V2 11029] LEA Suited Hydration
- [V2 11030] EVA Suited Hydration
Physiology
Spaceflight is associated with many factors which may affect crewmember urinary functions/health.
Urinary retention, renal stones, and UTIs are all identified as conditions that can be challenged by the
spaceflight environment and cause increased risk to crew health and mission outcomes.
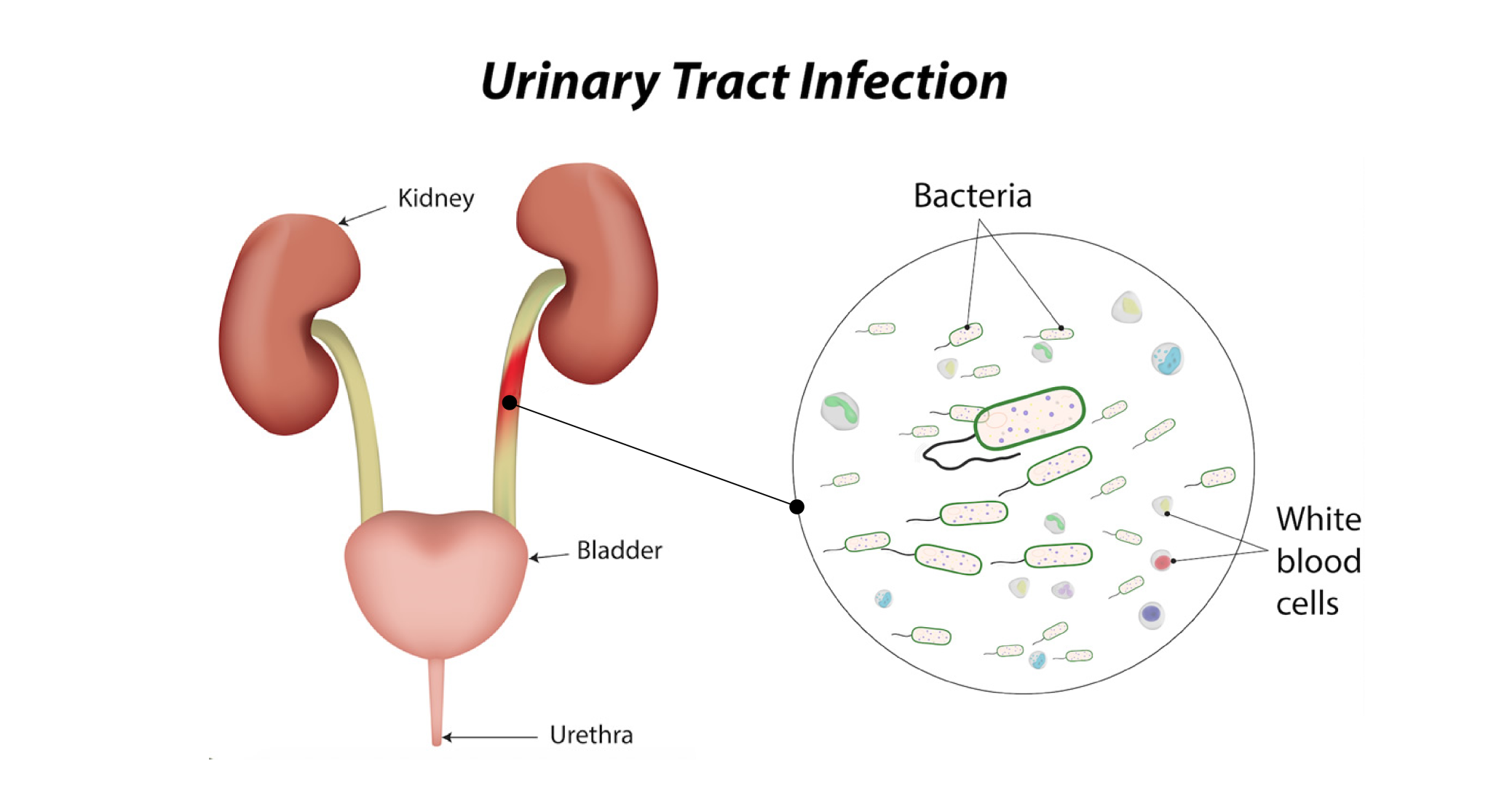
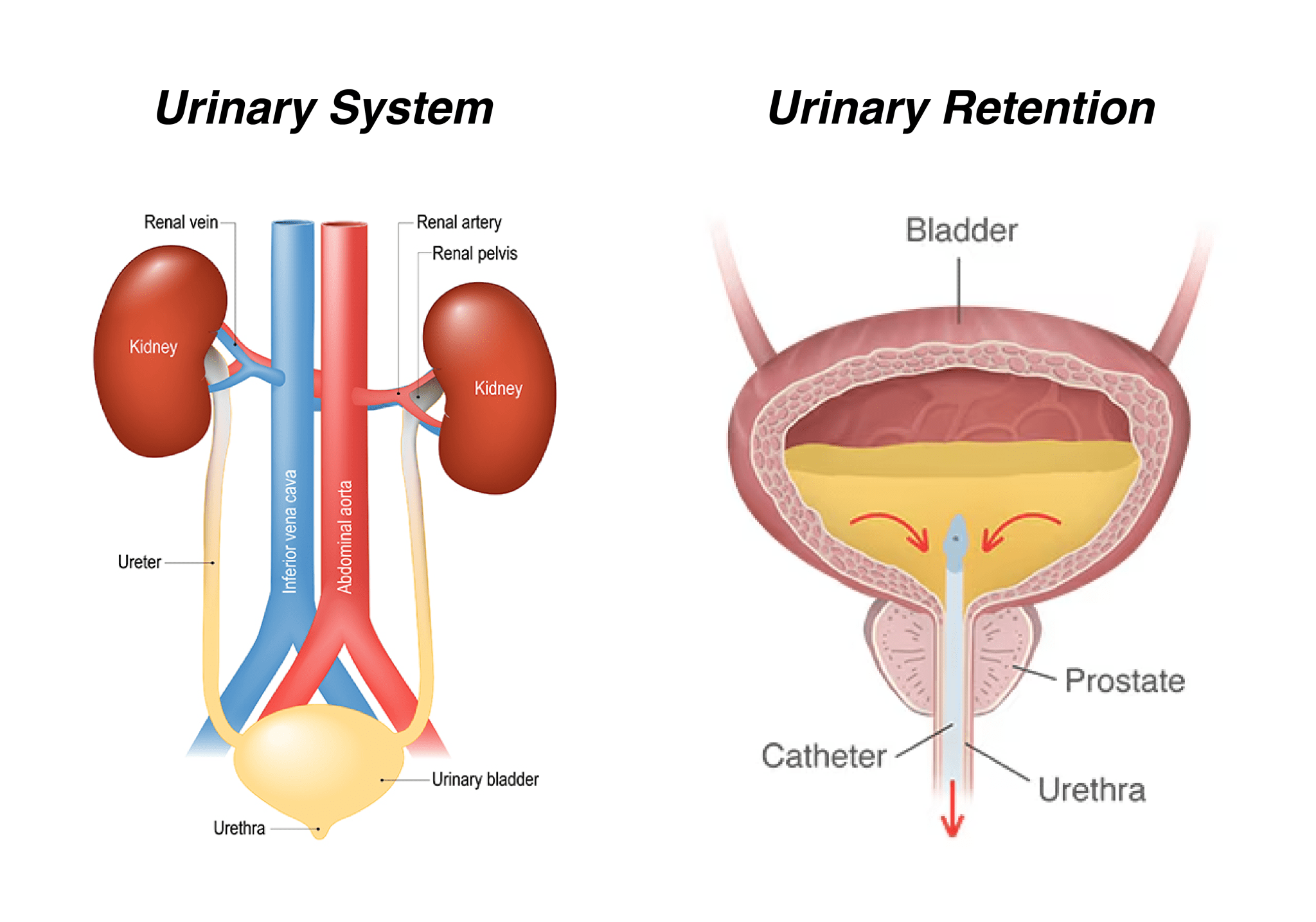
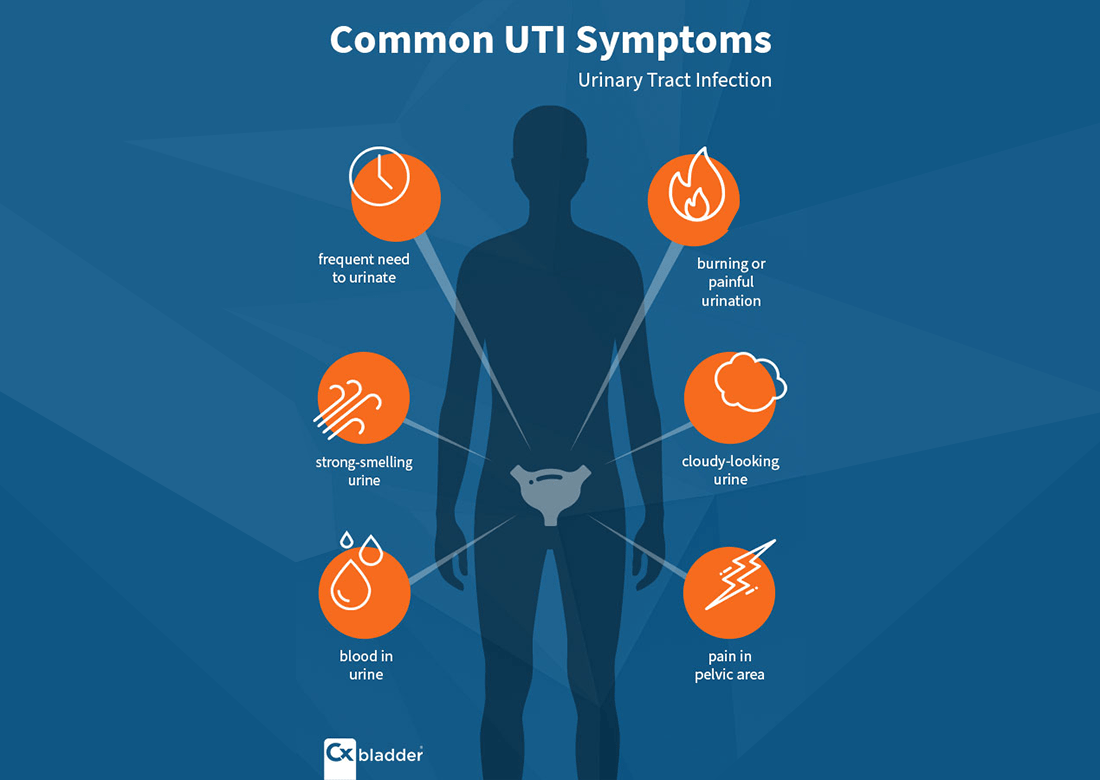
UTI : is a bacterial infection that occurs when bacteria enters the urinary tract and grows there. The urinary tract includes the kidneys, ureters, bladder, and urethra.
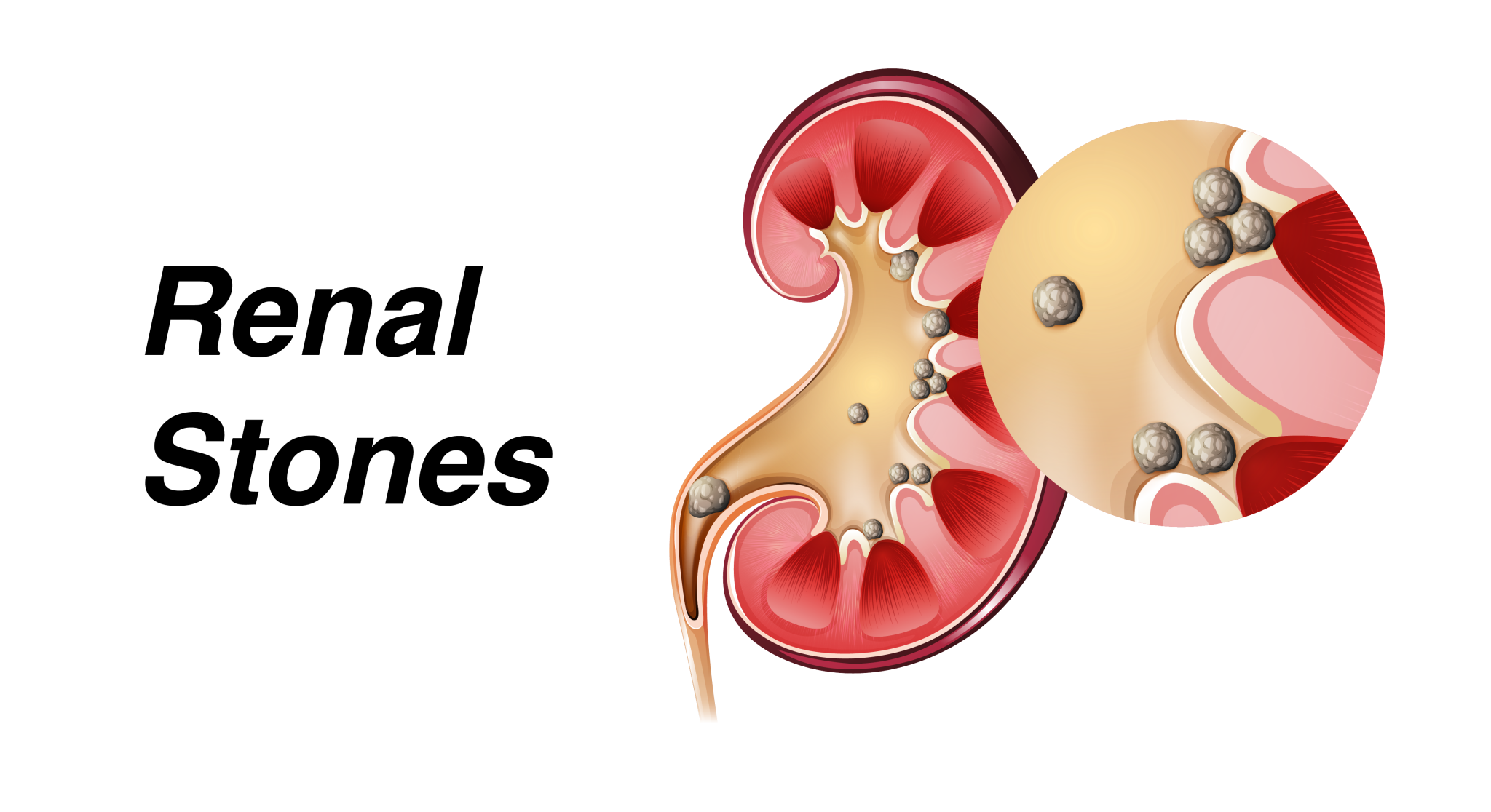
Renal stones : are aggregates of crystals that form in urine supersaturated in minerals, causing hard deposits in the kidneys.
Urinary Retention : is the inability, hesitancy, or difficulty in initiating urination.
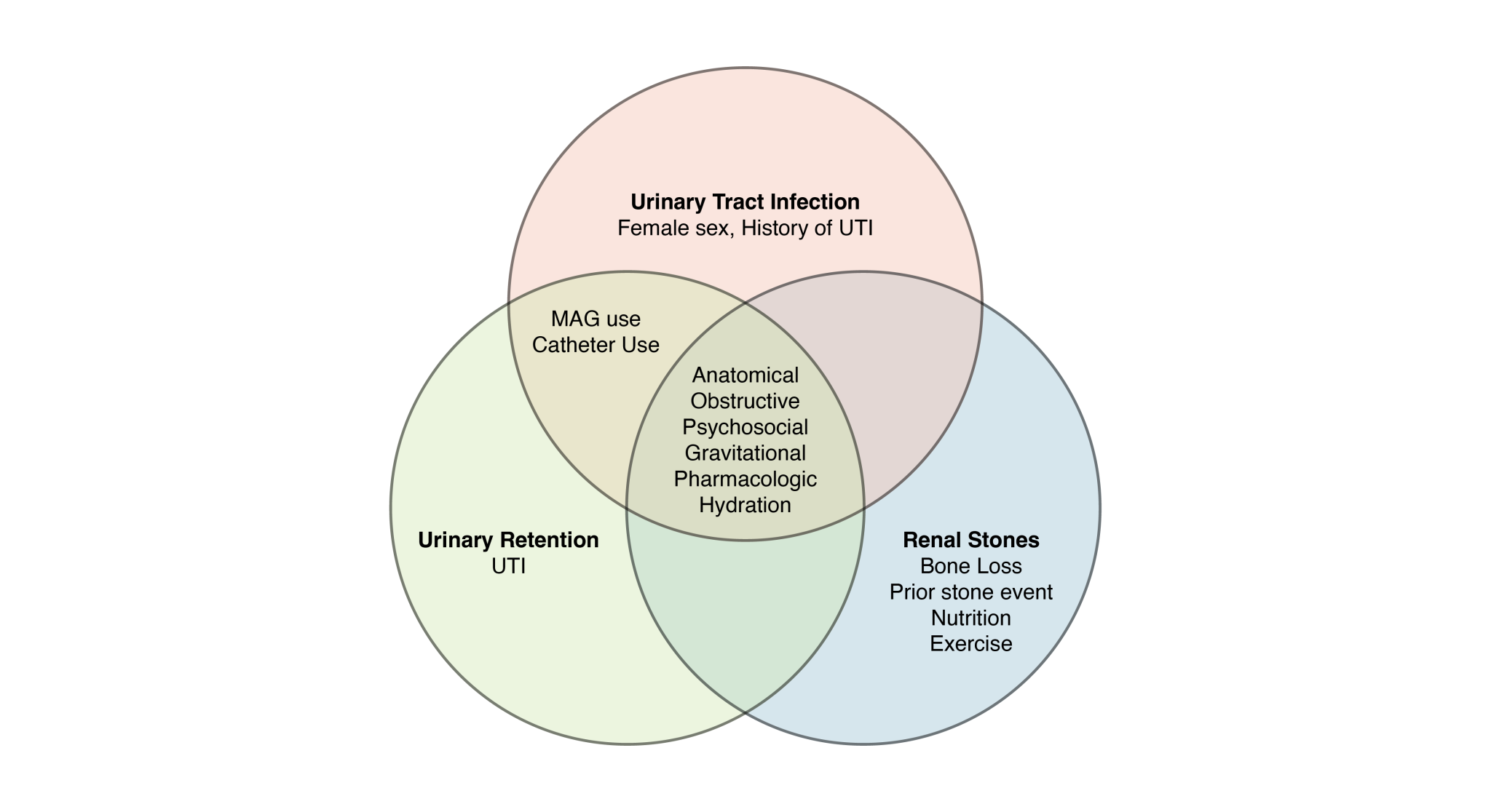
Spaceflight Urinary Health Factors
Anatomical/Physiological
- Male/Female
- Age
- Anatomical obstruction
- History of renal stones
- Psychosocial
- Neurogenic
- Bacterial infection/hygiene
Spaceflight Environment
- Gravitational effects
- Mission duration
- Mission conditions
- Bone loss
In-Mission Activity
- Catheter use
- Nutrition
- Pharmacologic
- Dehydration
- Exercise
- Use of Maximum Absorbency Garment (MAG)
Urinary Health Definitions
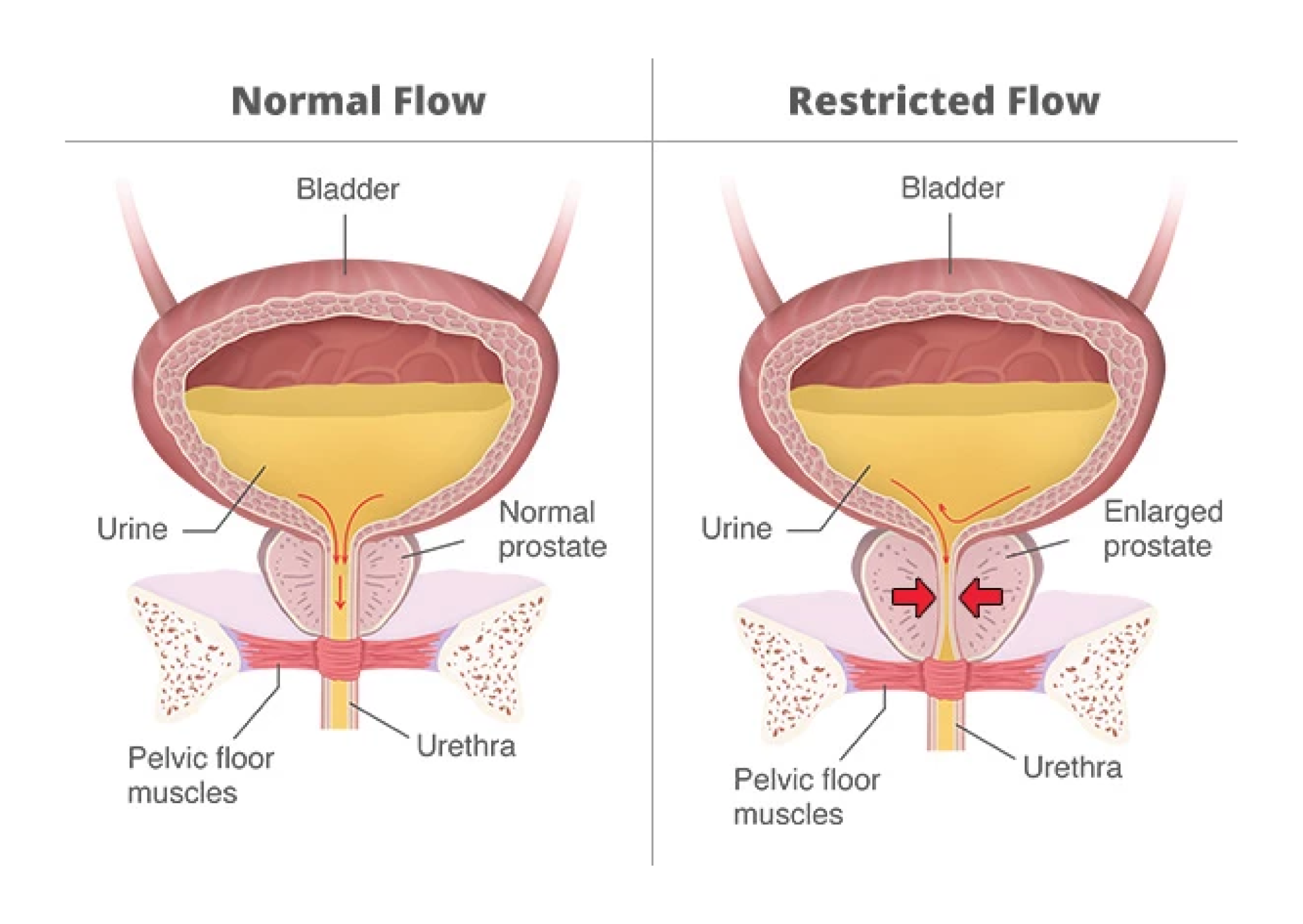
| Anatomical/obstructive | Female urethras make it easier for bacteria to enter the bladder due to urine splash back, especially when wearing a Maximum Absorbency Garment (MAG) or experiencing post-voiding urine. Male obstructive challenges include benign prostatic hyperplasia blocking urine flow and increased urinary retention. |
| Urine chemistry | Urine chemistry (calcium, potassium, citrate, oxalate and other substances) determines probability that Mineralized Renal Material (MRM) will precipitate from urine and increase stone risk. |
| Psychosocial effects | Crew may be hesitant to urinate or use MAG, especially at start of flight, leading to urinary retention and associated complications. |
| Maximum Absorbency Garment (MAG) | Diaper-like device that astronauts wear when they can’t take off their spacesuits for extended periods of time. MAGs are worn during liftoff, landing, and spacewalks. |
| Hydration | Water availability and intake affect risk of renal stones and UTIs. |
| Spaceflight bone loss | Lack of gravity (skeletal loading) can cause bone and calcium secretion into urine, increasing renal stone risk. |
| Gravity | Alterations in fluid dynamics and position of abdominal organs may increase risk of urinary retention. |
| Pharmacologic | Anticholinergic medications often used to prevent space adaptation sickness can interfere with normal bladder function causing urinary retention. |
| Nutrition | Nutrient intake of substances such as oxalate, calcium, magnesium, etc. affect urine chemistry. |
| Urinary Tract Infection (UTI) | Logistics of MAG use, catheter use, and toileting can increase exposure to bacteria and risk of UTI. Serious or untreated UTI can lead to sepsis. |
| Nephrolithiasis | Presence of crystalline stones (calculi) within the urinary tract. |
| Ureterolithiasis | Presence of calculi within the urinary system. |
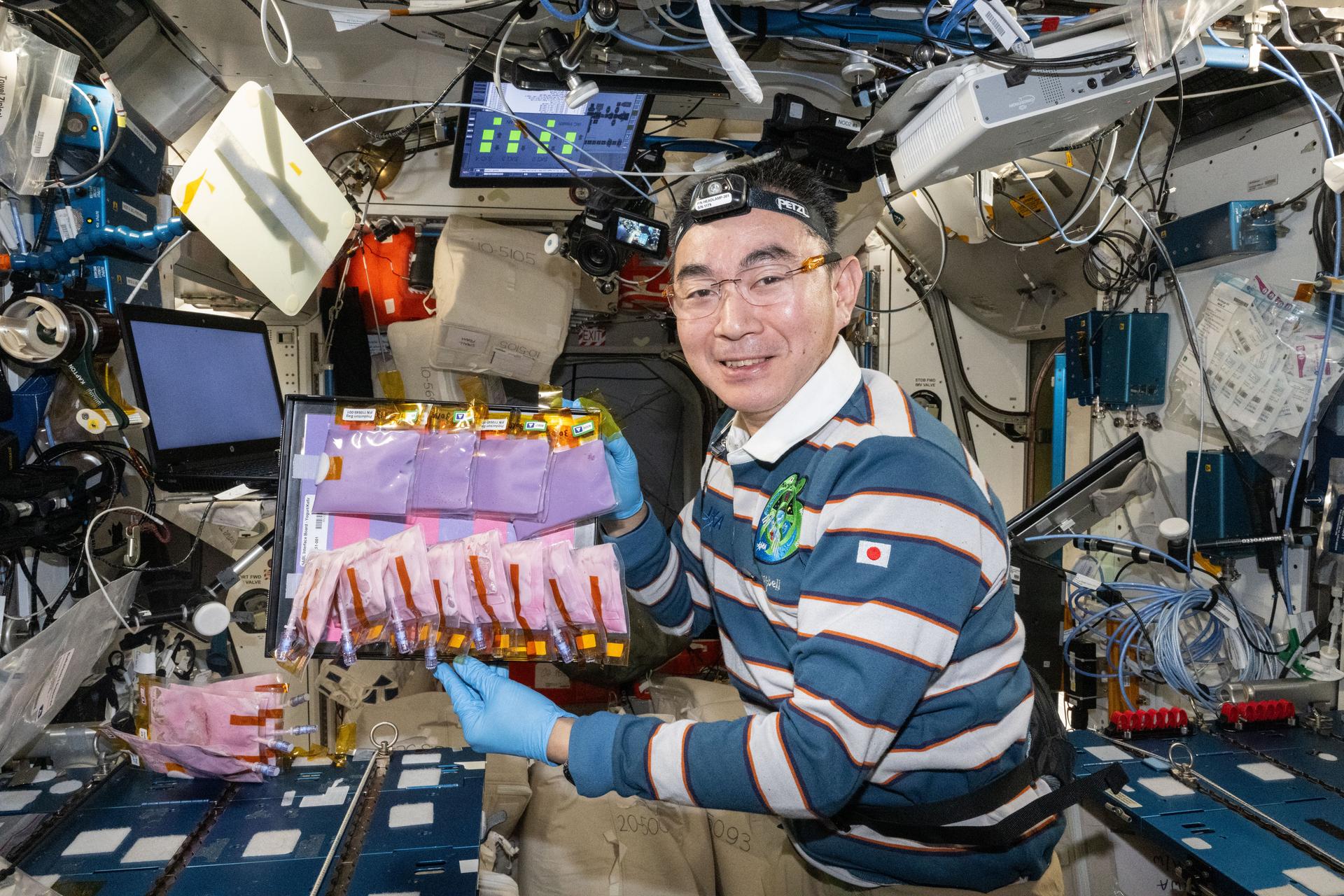
| Waste and hygiene compartment | Urine goes into hose, drawn by vacuum into disposal or recycling system. Toilet for solid waste consists of seat and bucket design with vacuum assist; waste is captured in plastic bag and closed after each waste event, can hold approximately 30 deposits. |
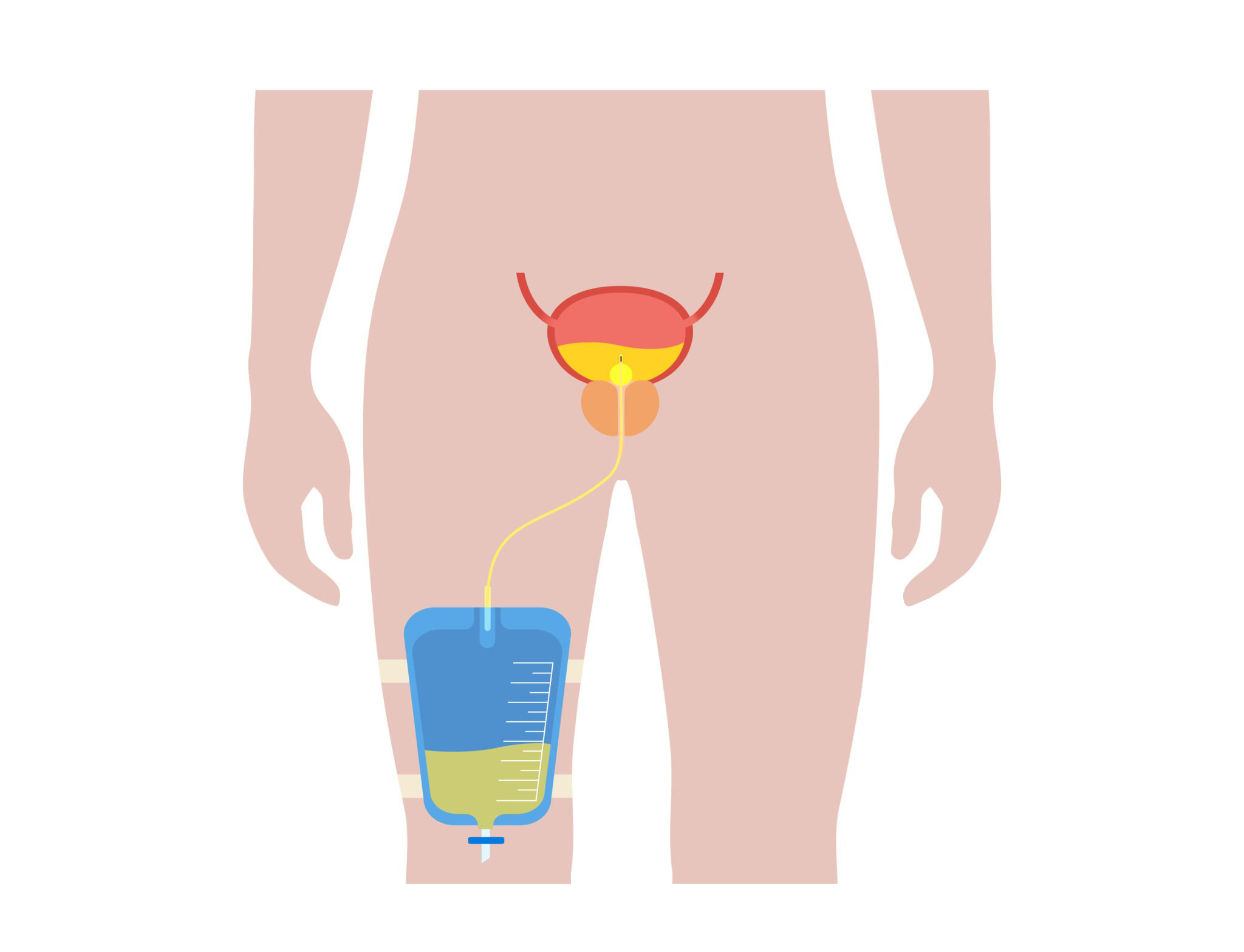
| Catheter | Crew can use catheters to treat urinary retention or other medical needs. Catheter use is associated with increased risk of UTIs. |
| Bladder obstruction | A physical condition that inhibits urine from flowing from the bladder. |
| Pyelonephritis/Sepsis | Pyelonephritis: UTI that affects one or both kidneys. Sepsis: life threatening condition when body’s immune systems overreacts to an infection, damaging body’s tissues and organs. |
| Post Void Residual (PVR) | Urine left in the bladder after voiding, possibly due to decreased sensation to void due to change in gravity vector. |
| Urine supersaturation | A condition caused by too much salt and insufficient fluid in the urine. |
Pathophysiology
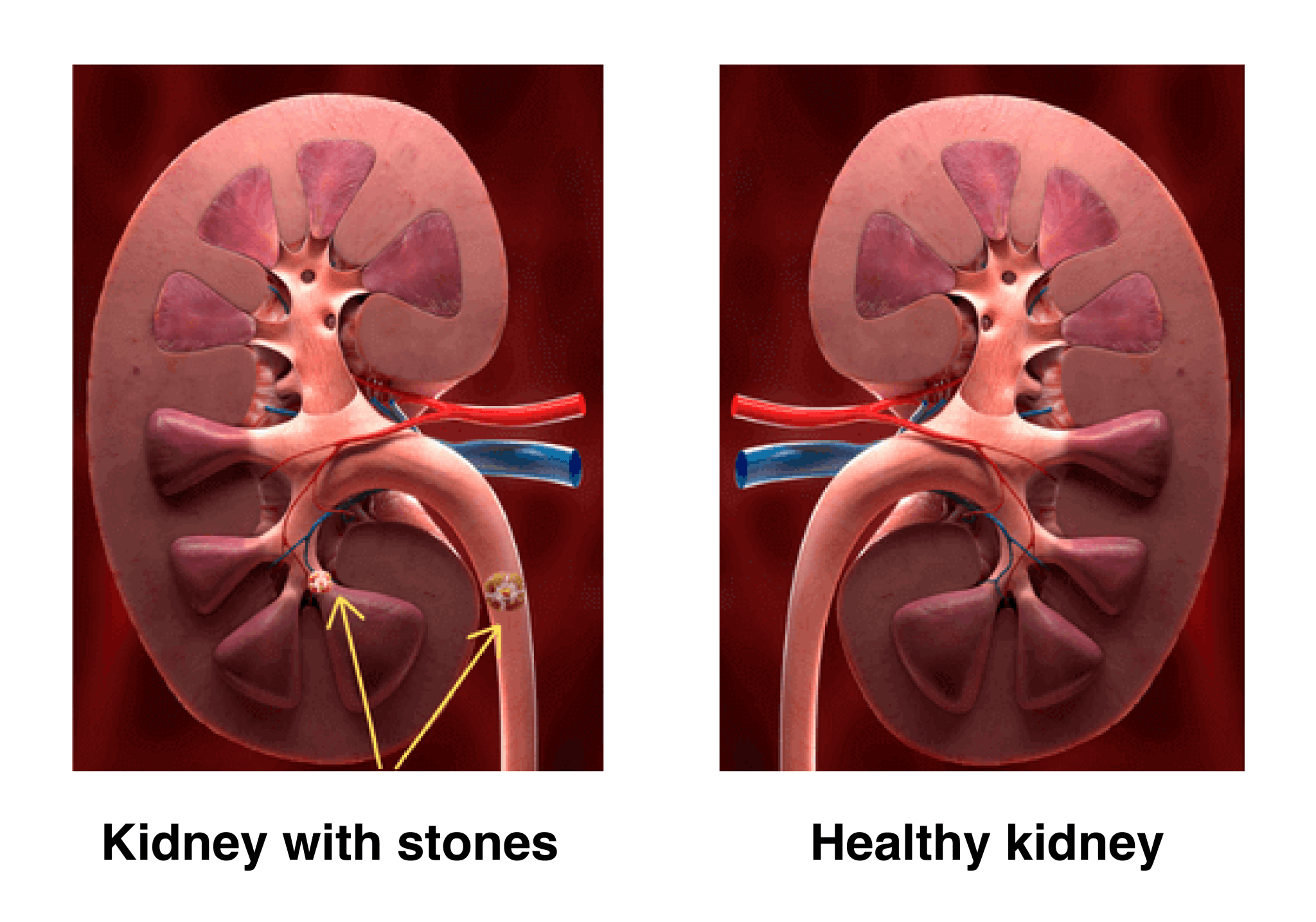
“Renal stones are aggregates of crystals formed in urine supersaturated in salt components, causing hard mineral deposits to occur in the kidneys. Renal stones are most often composed of calcium oxalate, uric acid, struvite, and cystine. Nephrolithiasis is the condition marked by development of renal stones.”
NASA HRP Evidence Report Risk of Renal Stone Formation
Terrestrial conditions that exacerbate renal stones
- Dietary: high animal protein/purine rich intake
- Dehydration: insufficient water intake
- Bone increases calcium excretion and
risk of calcium oxalate stones - Infections: UTIs change urine pH and increase risk of stones
- Family history
- Previous episodes: 60% will have reoccurrence
NASA STS-107 Space Research
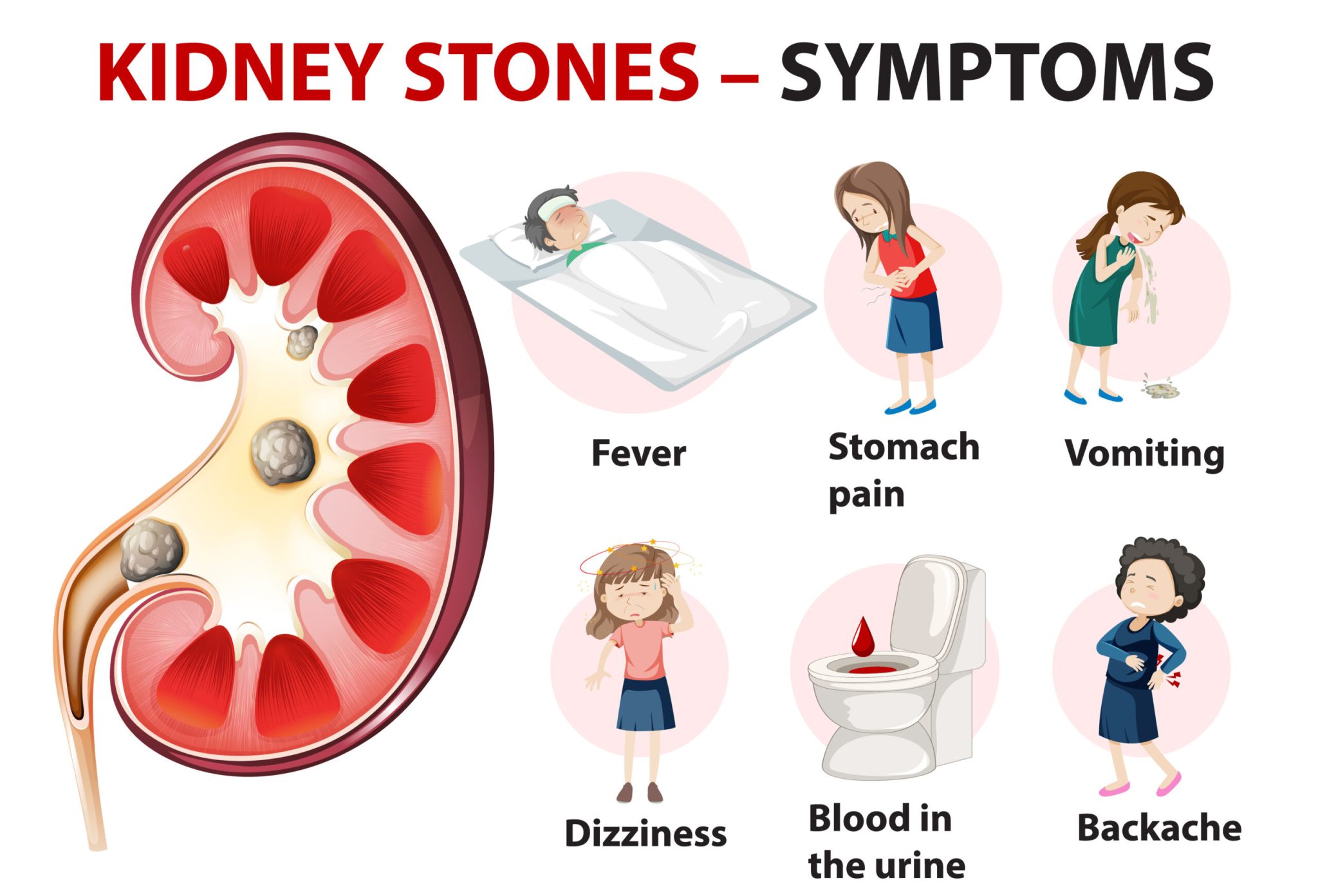
Renal stones are often small and go unnoticed, however stones become problematic when they increase in size causing pain, blocking the drainage of the kidney and urinary obstruction, affecting kidney function and increasing risk of UTIs. Potential complications include:
- Renal colic (pain)
- Hematuria (blood in urine)
- Infection/sepsis
- Hydronephrosis due to excess
backed up urine
Renal stone screening: History of renal stones were once a disqualifying condition for potential
astronauts. Currently, astronauts are individually evaluated and assessed with ultrasound/MRI prior to
flight. If evaluation determines an acceptable renal stone risk profile, they may be cleared to fly. The
protocol will be evaluated for longer duration moon/mars missions.
Risk of Renal Stone Formation “Given changes in urinary biochemistry during spaceflight, there is a
possibility that symptomatic renal stones will occur, which could cause renal colic (pain), nausea, vomiting,
hematuria, infection, and/or hydronephrosis.” NASA HSRB Renal Stone Risk (2022)
Spaceflight conditions that increase Renal Stone risk:
- Altered gravity/weightlessness increases bone resorption/loss and increases urinary calcium.
- Fluid changes including cephalad fluid shift.
- Decreased water intake (due to busy schedules and time-consuming logistics of urination).
- Changes in nutrient intake including high sodium and high animal protein.
- Changes in urinary PH and solute concentrations can affect urine chemistry.
Human Adaptation to Spaceflight: The Role of Food and Nutrition Scott et al.
Renal Stone Screening Profile: A renal stone risk profile is generated preflight based on urine volume
and chemistry. These data are used to determine the risk of supersaturation, which could lead to one or
more of several types of kidney stones.
Pre-flight Assessment: calcium oxalate, brushite, sodium urate, struvite, uric acid supersaturation
Pre/Post-flight Measurement: calcium oxalate, uric acid, citrate, pH, total volume, sodium, sulfate,
phosphorus, magnesium, potassium, creatinine
Monitoring/Management of Renal Stones Terrestrially, renal stones are detected using renal ultrasound,
CT imaging, and lab work including white blood count (indicates infection) and kidney function (creatinine,
blood urea nitrogen, and blood chemistries). Pre-flight and post-flight renal ultrasound are standard. If
renal stones are suspected in-flight, ultrasound and limited lab work can detect and help enable stone risk
management. Promising technology (ex. propulsive ultrasound, burst wave lithotripsy) is being studied for
the possibility of manipulation of stones, moving or breaking them up to assist with in-flight stone
elimination or symptom reduction.
To date there has been one reported episode of nephrolithiasis during spaceflight; a cosmonaut
experienced severe lower abdominal pain that spontaneously resolved. No USOS crewmembers have
reported kidney stones while in flight. A total of 43 stone events in 29 crewmembers have been recorded
by NASA since 2016. NASA Evidence Report Risk of Renal Stone Formation HRP ExMC 2017, NASA HSRB
Renal stone Risk package LSAH Surveillance Data 2022
Urinary Tract Stone Events in the Astronaut Corps
| Time | Total # of Events | Comments |
|---|---|---|
| Before Flight | 5 | Stone discovered before any mission |
| 0-90 days after spaceflight | 1 (1) | |
| 90-180 days after spaceflight | 3 (1) | |
| 180-270 days after spaceflight | 1 | |
| 270-360 days after spaceflight | 2 | |
| Between Flights | 4 (1) | >360 days after mission but prior to next mission |
| Post Flight Career | 26(1) | >360 days, did not fly again |
| Total | 43(4) |
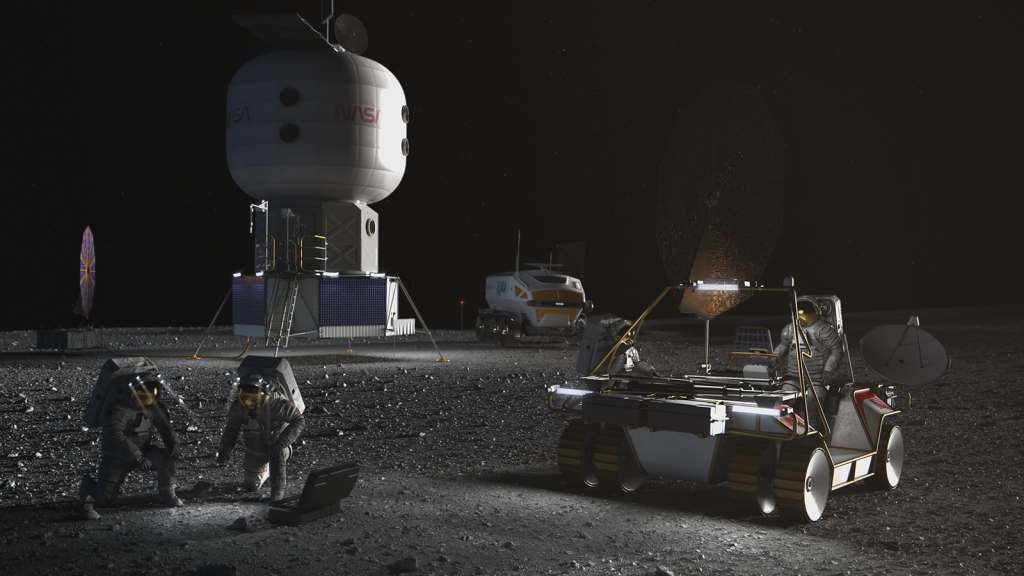
Toilet design and toileting challenges (shown above) can contribute to urinary retention and urinary
tract infection risk during spaceflight.
How to use the Bathroom in Space
NASA’s Chris Cassidy explains some of the
challenges of toilet design in space
Countermeasures/Treatment for Renal Stones:
- Pre-flight screening and selection measures detect problems prior to flight.
- Hydration – ensure crew has ample supply of water and is encouraged to drink an adequate amount.
- Exercise can preserve bone mineral density, decreasing the amount of stone forming calcium in urine.
- Manage the amount of stone forming substances including oxalate, calcium, magnesium, and salt
contained in food. - Pharmaceuticals – potassium citrate (Kcit) (Whitson et al., 2009) and
thiazide (Reilly et al., 2010) directly affect urine chemistry and can prevent
stone formation; bisphosphonates can affect bone remodeling and decrease
calcium released into blood (Leblanc et al., 2013). - Tamsulosin can relax ureter smooth muscle and allow stones to pass faster
(Cui et al., 2019), NSAIDS and opioids can assist with stone pain, ondansetron
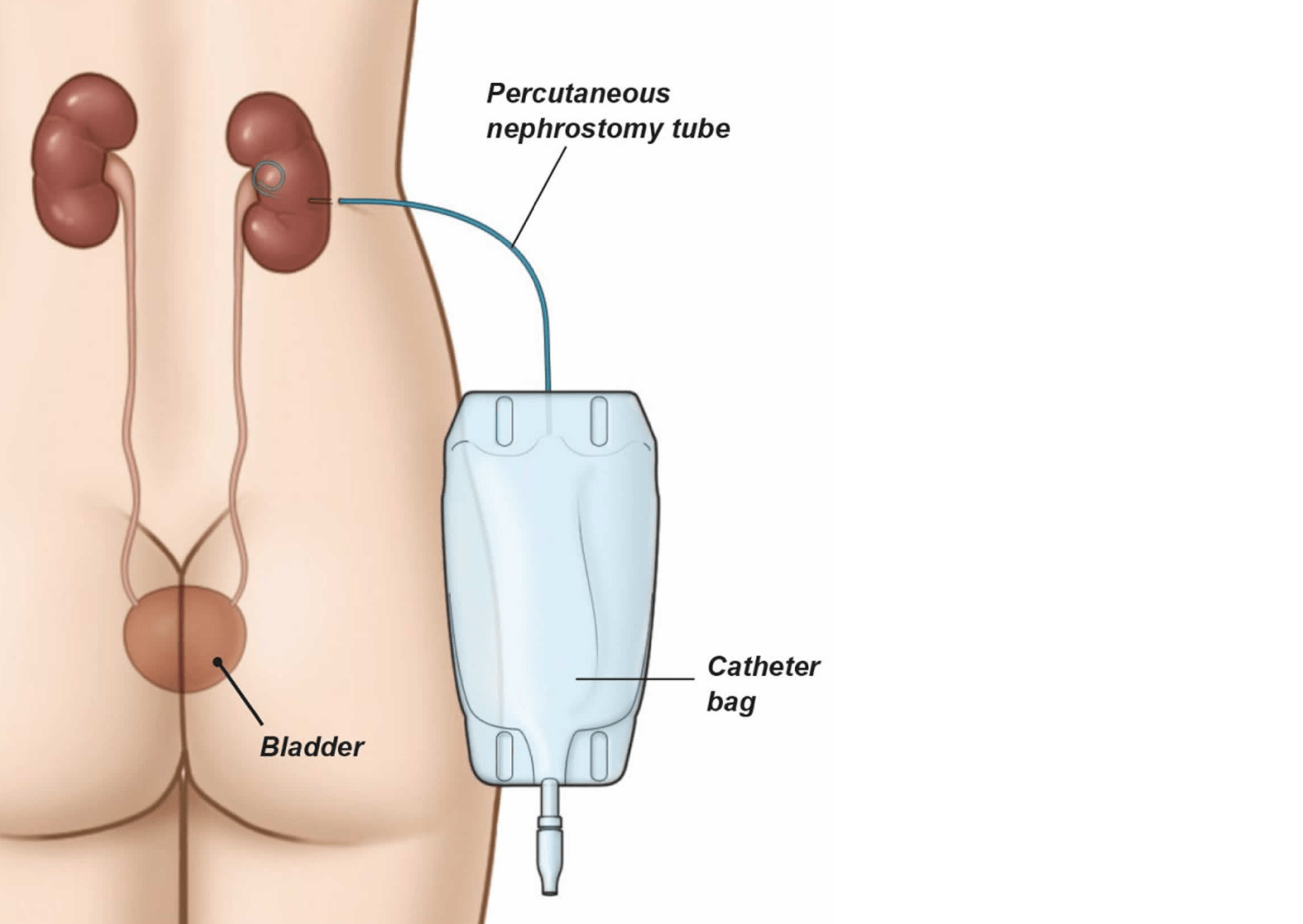
can assist with nausea associated with stone pain. - Catheter/nephrostomy tube can be used in cases of urinary retention to help drain fluid that is blocked.
Potassium Citrate (KCit) : provides an alkali influence, increasing urinary PH, decreasing urinary calcium
excretion and calcium oxalate supersaturation, ultimately decreasing risk of renal stones. KCit and
potassium magnesium citrate supplements have successfully reduced the number of incidents of renal
stones during bed rest, KCit is now available on ISS for use at the flight surgeon’s discretion if clinically
indicated. The size and potential volume of KCit tablets for an astronaut crew is a challenge to
spaceflight programs. Whitson 2009.
Bisphosphonates : inhibit osteoclastic bone resorption and increase osteoclast apoptosis which
decreases bone breakdown, decreasing calcium in urine and ultimately renal stones. Bisphosphonates
have been studied in long-duration astronauts and the data collected from these studies suggest that
this class of drug reduces the loss of trabecular bone mineral density and helps preserve total bone mass
in space as well as prevent hypercalciuria (and renal stone formation). Bisphosphonates are associated
with significant side effects including osteonecrosis of the jaw (ONJ), atypical femur fractures,
esophageal complications, and kidney changes. (Rosenthal 2024)
Water Quantities and Temperatures
| Requirment | Quantity | Hot Temperature | Nominal Temperature | Cold Temperature |
|---|---|---|---|---|
| Potable Water for Hydration | Minimum 2.5 L per crewmember | Between 68 °C – 79°C | Between 18 °C – 27 °C | Maximum temp of 16 °C |
| Potable Water for EVA Operations | Minimum 240 ml per crewmember /EVA hour | Between 68 °C – 79°C | Between 18°C –27 °C | Maximum temp of 16 °C |
Hydration is a countermeasure to Renal Stones supported by: Water Quantity [V2 6109]
The system shall provide a minimum water quantity as specified in the Table (modified left), for expected needs of each mission, considered mutually independent.
Urinary Retention is the impaired ability to urinate due to mechanical or functional obstruction of urinary
tract, including hesitancy or difficulty to initiate urination.
Urinary Retention Predisposing Factors 9 cases of urinary retention have been documented during spaceflight-the potential causes include:
- Obstructive (anatomical) i.e., enlarged prostate
- Psychosocial – retention due to schedule and toilet access i.e., not wanting to use MAG
- Infection (UTI)
- Altered Gravity Vector – Post Void Residual (PVR) is urine left in the bladder after voiding. PVR may be due to decreased sensation to void due to change in gravity vector. PVR is not considered urinary retention but can lead to UTI and retention
- Pharmacologic – anticholinergic use
- Radiation, hostile closed environment, and isolation and confinement can increase inflammation which can increase risk
- Urinary muscle changes that occur in altered gravity environments
- Age, sex, and genetic predisposition
- Retention risk increased on post-flight day 1; this could impact planetary missions upon landing on
celestial bodies
| P<0.01 | Retention Rate | 95% Confidence Limits | |
|---|---|---|---|
| Female | 0.0510 | 0.0217 | 0.1151 |
| Male | 0.0111 | 0.0053 | 0.0230 |
- The odds of developing urinary retention inflight are 4.5x higher among female astronauts, which is very different from terrestrial data and may be attributed to the altered gravity vector, limited bathroom facilities, MAG use, and psychosocial factors.
- Terrestrially, urinary retention ratio is 10 Male to 1 Female. Urinary retention in men becomes more common with age, often related to prostate gland issues.
- Other causes (independent of gender) include neoplasms, trauma, acute inflammation, damage to nerves that supply the bladder, and spinal cord trauma (neurogenic retention)
Management of lower urinary retention in a limited resource setting. Ugare et al.
The higher prevalence of spaceflight urinary retention in females is even more concerning given that there have been many more males in space than females.
| Shuttle | ISS | Catheter Required | EVA Related | SMS Med Usage | |
|---|---|---|---|---|---|
| Urinary Retention | 8 | 1 | 4 | 1 | 7 |
| Bladder fullness/pressure | 2 | 0 | 0 | 0 | 1 |
| Difficulty initiating/hesitancy | 5 | 0 | 0 | 1 | 4 |
| TOTAL | 15 | 1 | 4 | 2 | 12 |
NASA Risk of Urinary Retention : Given that the spaceflight environment alters the gravity vector involved in terrestrial urination and causes physiological changes that may require use of medications, and that mission operational schedules may limit access to voiding, there is a possibility of performance impact during spaceflight due to significant discomfort from urinary retention and associated UTI. Symptomatic urinary retention happens in flight and on landing day.
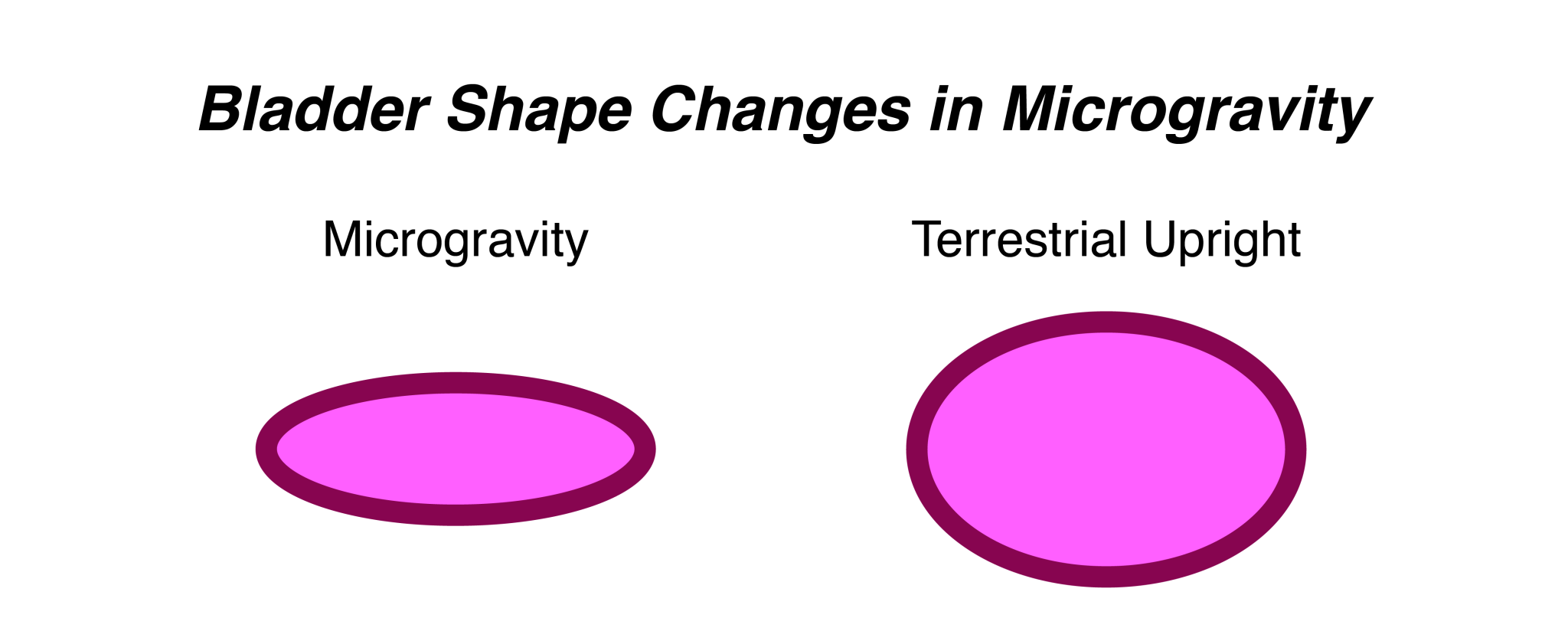
Bladder physiology in space : The lack of gravity influences the urine in the bladder. Terrestrially, urine collects at the bladder neck, while in space it adheres to the bladder wall. The surface tension is the major force for the urine, thus the sensation for urination triggers only when the bladder is completely full. In the continuation, negative pressure helps capillary action for the urine transport from the bladder to the outward.
The Place of Urology in Aerospace Medicine Mar 2022
Consequences of urinary retention : UTIs, pyelonephritis (kidney infection), and potentially sepsis if untreated. Renal colic, retention pain, and hydronephrosis can result from urinary retention or urine flow disruption. All of these if untreated can potentially lead to acute renal failure with implications for evacuation, loss of crew life, and long-term health issues including permanent bladder dysfunction and long-term renal failure.
Countermeasures and Treatment:
- Catheter use
- Pharmacologic – tamsulosin increases urine flow
- Percutaneous bladder catheterization – has been studied but to date has not been used
Catheter use challenges : “To perform the procedure requires training and maintenance of proficiency, adequate supplies including disinfection swabs, lubricant, catheters, and collection devices. A private environment, patient ability to lie flat can be complicated by microgravity or aircraft ferrying a post-flight crewmember. The procedure can be time-consuming negatively impacting tight operational schedules.”
Law & Cardy (2023) Pharmacological relief of acute urinary retention in a remote environment.
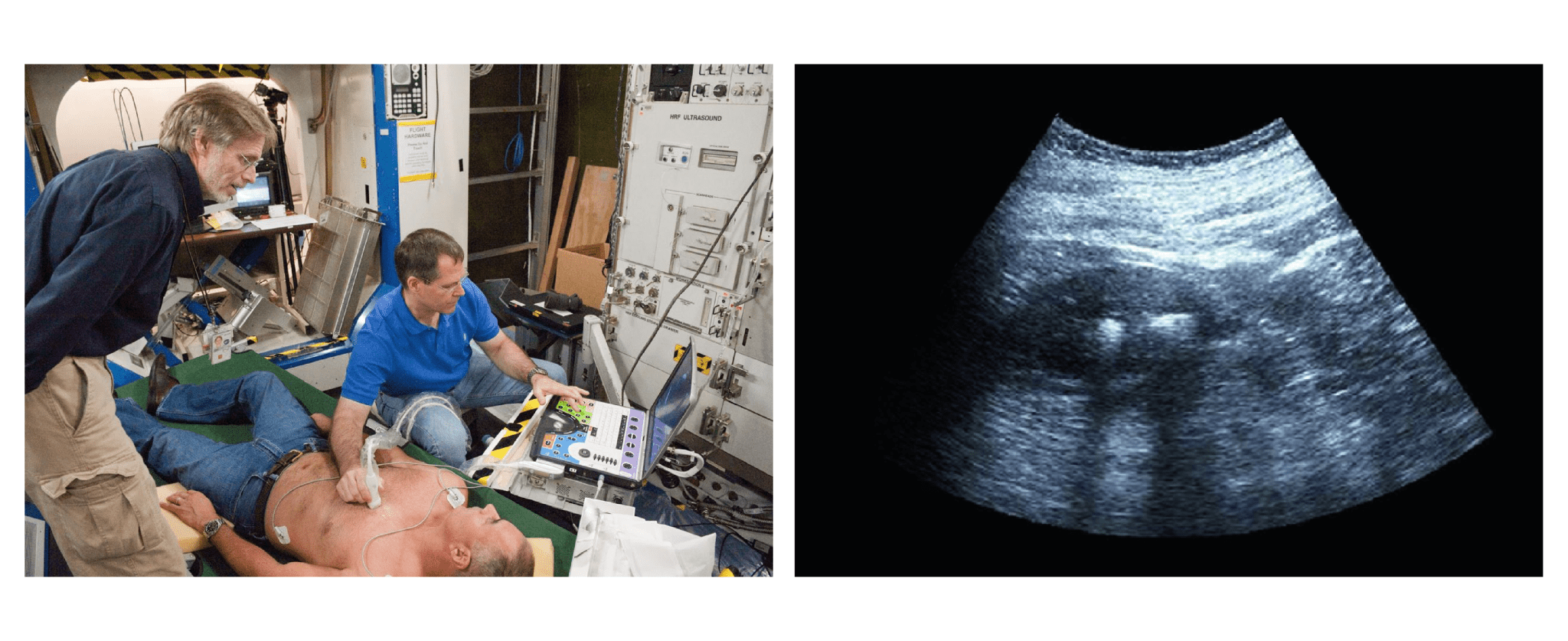
Percutaneous bladder catheterization : and drainage can be successfully performed in weightless conditions under ultrasound guidance. Ultrasound provides a low-power, portable means to safely guide minimally invasive procedures in pertinent organs and tissues. Percutaneous bladder catheterization is a standard procedure when luminal bladder catheterization is not possible; this technique can be successfully modified for use in space medicine applications. Percutaneous bladder catheterization in microgravity Jeffrey A. Jones et al.
Catheter use can increase risk of UTI. Once an indwelling catheter is placed, the daily incidence of bacteriuria is 3-10%
A urinary tract infection (UTI) : is a bacterial infection that occurs in the urinary tract, including kidneys, ureters, bladder or urethra. Among all medical conditions, infections pose one of the biggest threats to astronaut health and mission success. UTIs are caused from bacteria, often from the large intestine traveling from the anus or other exposure to genital area skin, then into the urethra, bladder, and potentially kidneys if not treated early enough. Females are more susceptible to UTIs due to their shorter urethra. The toileting conditions of spaceflight cause increased exposure to bacteria from wearing a MAG, PVR, and limited space in the toilet area making usual cleaning more difficult. In addition, urinary retention is treated with catheterization which increases risk of UTIs.
UTI Countermeasures and Treatment :
- Antibiotics are the treatment of choice for UTI.
- Training and practice of proper aseptic technique as well as pre medicating crew when wearing catheters can assist with UTI prevention.
- Prophylactic antibiotic use can be considered, especially in susceptible patients or patients with
catheter use. - Hydration– staying hydrated can help prevent conditions that favor UTI development.
- Analgesics can help with pain/discomfort associated with UTI.
Possible challenges to antibiotics in space :
- Medication supplies can become depleted, shelf live issues and potentially decreased antibiotic
effectiveness - Potential for bacterial resistance
- Theoretical increased pathogen virulence
- Altered immune function
- Inadequately treated UTI may lead to pyelonephritis and sepsis evacuation or mission impact
Maximum Absorbency Garment (MAG)
Using the MAG, especially for long duration exposure can cause irritation to the skin and increase urinary
tract infection risk. The Orion contingency plan in the event of a depressed cabin is to spend a maximum of
144 hours in the suit, although a purpose-built waste contingency system is used instead of MAGs.
Application
Apollo 13 Fred Haise
Fred Haise developed a serious UTI during Apollo 13. Haise became increasingly unwell during the last 4 days of the mission and was feverish during the final day. It is speculated that he developed a UTI, possibly from catheter use and the bacteria, Pseudomonas aeruginosa, spread to his kidneys, causing intense pain and threatening to infect other parts of his body.
Pseudomonas is an opportunistic pathogen that has difficulty infecting healthy people. However, astronaut bodies are under a lot of stress. For example, microgravity changes the way fluids distribute in the body and affects immune function. Additionally, on Apollo 13, Haise was faced with significant additional mental and physical stresses. Crammed into the Lunar Module after the Command Module lost power, he endured freezing temperatures and was dehydrated from water rationing, all while facing the very real possibility of not making it home.
“Numerous factors could have increased Haise’s susceptibility to infection, including potential changes in the behavior of the pathogen itself and how it interacted with Haise’s own suite of microorganisms—his microbiome. A growing body of evidence suggests that some microbes behave differently in space than on Earth, and space travel alters the microbiome of astronauts in ways not yet completely understood. Although Haise survived and had no lasting effects, a longer flight may have had grim consequences.” Microbial Hitchhiker’s Guide to the Galaxy: Researchers race to understand effects of deep space on microbiome
NASA is researching the impact of space flight on pathogens to better understand their impact to crew, helping to prepare us for longer spaceflight, including multi year missions to mars, which will pose new and unknown challenges to crew health.
Haise was treated with an antibiotic and made a complete recovery after landing. It is suspected that the
infection could have become debilitating if the mission had lasted much longer.
Source: Apollo Journal
Reference List
- National Institutes of Health (NIH) NIDDK. Definition & Factors of Urinary Retention. Available at:
https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-retention/definition-facts - Law, J, Cole, R, Young, M, & Mason, S. (2016). NASA Astronaut Urinary Conditions Associated with
Spaceflight. JSC-CN-34668. - Sibonga, JD, & Piertzyk, R. (2017). Evidence Report: Risk of Renal Stone Formation. JSC-CN-39600.
- Okada, A, et al. (2021). Bisphosphonate Use May Reduce the Risk of Urolithiasis in Astronauts on
Long-Term Spaceflights. JBMR Plus, 22:6(1): e10550. - Woods, D, Kemppanen, J, Turhanov, A, & Waugh, LJ. (2020). Apollo 13 Flight Journal. Available at:
https://www.nasa.gov/history/afj/ap13fj/index.html - Wilson, N. (2019). A Microbial Hitchhiker’s Guide to the Galaxy: Researchers race to understand effects
of deep space on microbiome. BioScience, 69(1): 5-11. - Baran, C, Erkoc, M, & Otunctemur, A. (2022). The Place of Urology in Aerospace Medicine: A New
Horizon. European Archives of Medical Research, 38(1): 1-4. - Stratton, E, Reyes, D, & Cole, R. (2024). Evolution of Spaceflight Renal Stone Risks and Update to the
NASA Human Research Program (HRP) Renal Stone Evidence Report and Integrated Concept of
Operations. - NASA Space Science Research. (2002). STS-107 Shuttle Press Kit. Available at:
https://www.nasa.gov/wp-content/uploads/2023/05/2222main-sts-107-presskit.pdf?emrc=b12820 - Stepaniak, PC, Ramchandani, SR, & Jones, JA. (2007). Acute urinary retention among astronauts. Aviat
Space Environ Med, 78(4): 5-8. - Jones, JA, Jennings, R, Pietryzk, R, Ciftcioglu, N, & Stepaniak, P. (2005). Genitourinary Issues during
spaceflight: a review. Int J Impot Res, 17(Suppl 1): S64-7. - Jones, JA, Kirkpatrick, A, Hamilton, DR, Sargsyan, AE, Campbell, M, Melton, S, Barr, YR, & Dulchavsky,
SA. Percutaneous Bladder Catheterization in Microgravity. Can J Urol, 14(2): 3493-8. - Nojaba, L, & Guzman, N. (2023). Nephrolithiasis (Kidney Stones). StatPearls [Internet].
- Zerwekh, JE, Odvina, CV, Wuermser, LA, & Pak, CYC. (2007). Reduction of renal stone risk by
potassium-magnesium citrate during 5 weeks of bed rest. J Urol, 177(6): 2179-2184. - Ugare, UG, Bassey, IA, Udosen, EJ, Essiet, A, Bassey, OO. (2014). Management of Lower Urinary
Retention in a Limited Resource Setting. Ethiop J Health Sci, 24(4): 329-336. - Whitson, PA, Pietrzyk, RA, & Sams, CF. (2001). Urine volume and its effects on renal stone risk in
astronauts. Aviat Space Environ Med, 72(4):368-72. 18. - Law J, & Cardy V. (2023). Pharmacological relief of acute urinary retention in a remote environment.
Aerosp Med Hum Perform, 94(2):90–93. - Jones, JA, Kirkpatrick, AW, Hamilton, DR, Sargsyan, AE, Campbell, M, Melton, S, Barr, YR, & Dulchavsky,
SA. (2007). Percutaneous bladder catheterization in microgravity. Can J Urol, 14(2): 3493-8. - Stratton, E, Lumpkins, S, & Antonsen, E. (2024). Evidence Report: Risk of Renal Stone Formation
Human Research Program, Exploration Medical Capabilities Element. - Mayo Clinic Diseases and Conditions: Kidney stones. Available at:
https://www.mayoclinic.org/diseases-conditions/kidney-stones/symptoms-causes/syc-20355755. - Kassemi, M, & Thompson, D. (2016). Prediction of renal crystalline size distributions in space using
a PBE analytic model. 2. Effect of dietary countermeasures. Am J Physiol Renal Physiol, 311(3):
F520-30. - Simon, JC, et al. (2018). Renal on flexible ultrasound – imaging technologies. Available at:
https://www.nasa.gov/wp-content/uploads/2018/04/renal_on_flexible_ultrasound-_j._simon.pdf?emrc=4165d6 - Goodenow-Messman, DA, Gokoglu, SA, Kassemi, M, & Meyers, JG. (2022). Numerical
characterization of astronaut CaOx renal stone incidence rates to quantify in-flight and post-flight
relative risk. npj Microgravity, 8(2). - NASA HSRB Renal Stone Risk 2022
- Stratton et al NASA Evidence Report : Risk of Renal Stone Formation 2024
- Barratt et all Principles of Clinical Medicine for Space Flight 2nd edition 2019
- Whitson PA, Pietrzyk RA, Jones JA, Nelman-Gonzalez M, Hudson EK, Sams CF. Effect of potassium
citrate therapy on the risk of renal stone formation during spaceflight. J Urol. 2009 Nov;182(5):2490- - doi: 10.1016/j.juro.2009.07.010. Epub 2009 Sep 17. PMID: 19765769.
- Pietrzyk RA, Jones JA, Sams CF, Whitson PA. Renal stone formation among astronauts. Aviat Space
Environ Med. 2007 Apr;78(4 Suppl):A9-13. PMID: 17511294. - Niki Wilson, A Microbial Hitchhiker’s Guide to the Galaxy, Bioscience Dec 2018. Doi
10.1093/biosci/biy140, pub.1110070035