Small devices that mimic functions of human organs help researchers understand the progression of various diseases and provide a faster and safer alternative to preparing drugs for clinical trials.
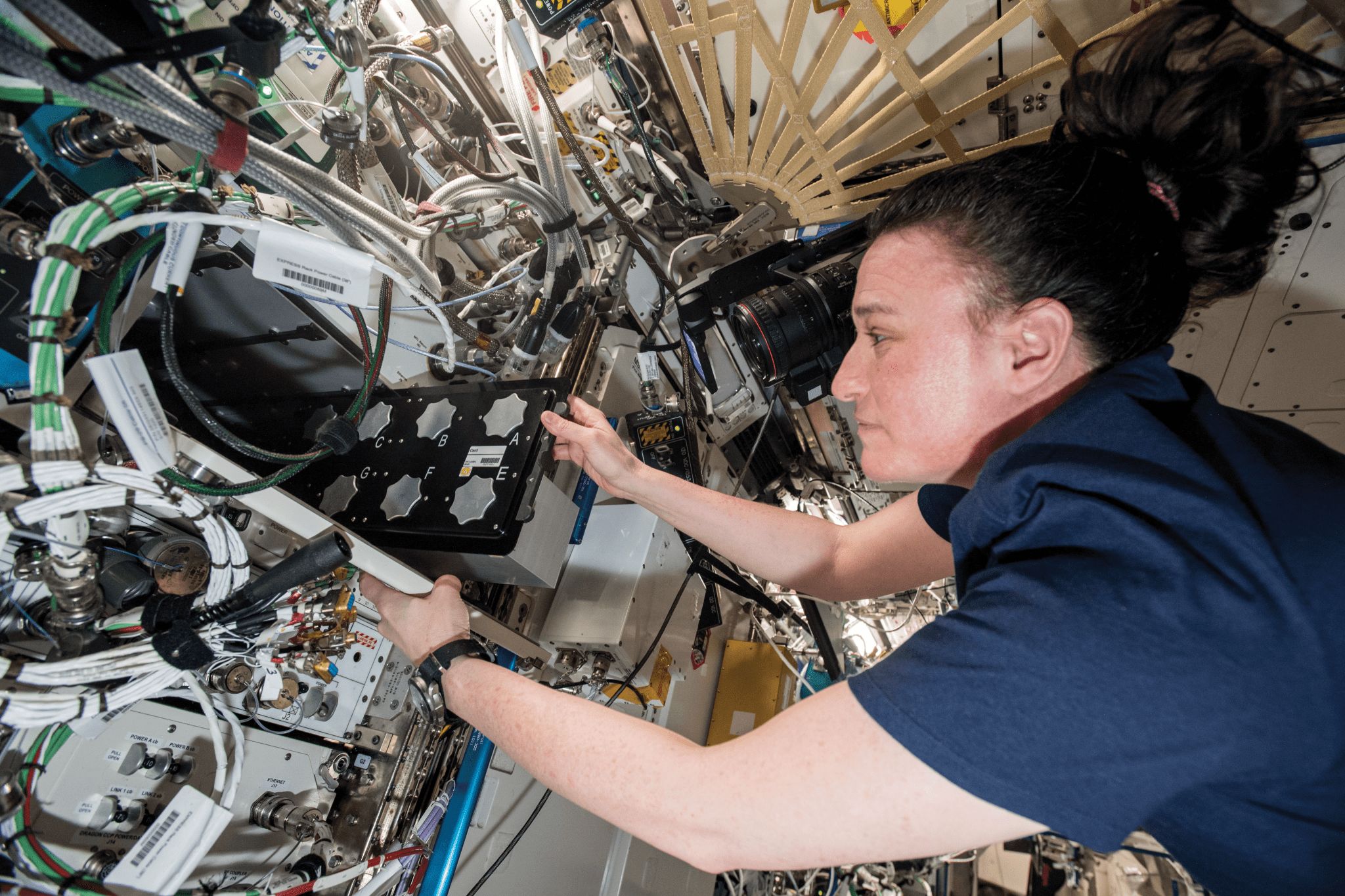
Tiny canisters of beating human heart cells that flew on the International Space Station could help scientists understand abnormalities in heart cells and tissues that can lead to disease on Earth. The Cardinal Heart investigation used these engineered heart tissues (EHTs), a type of tissue chip, to examine how microgravity affects heart cells.
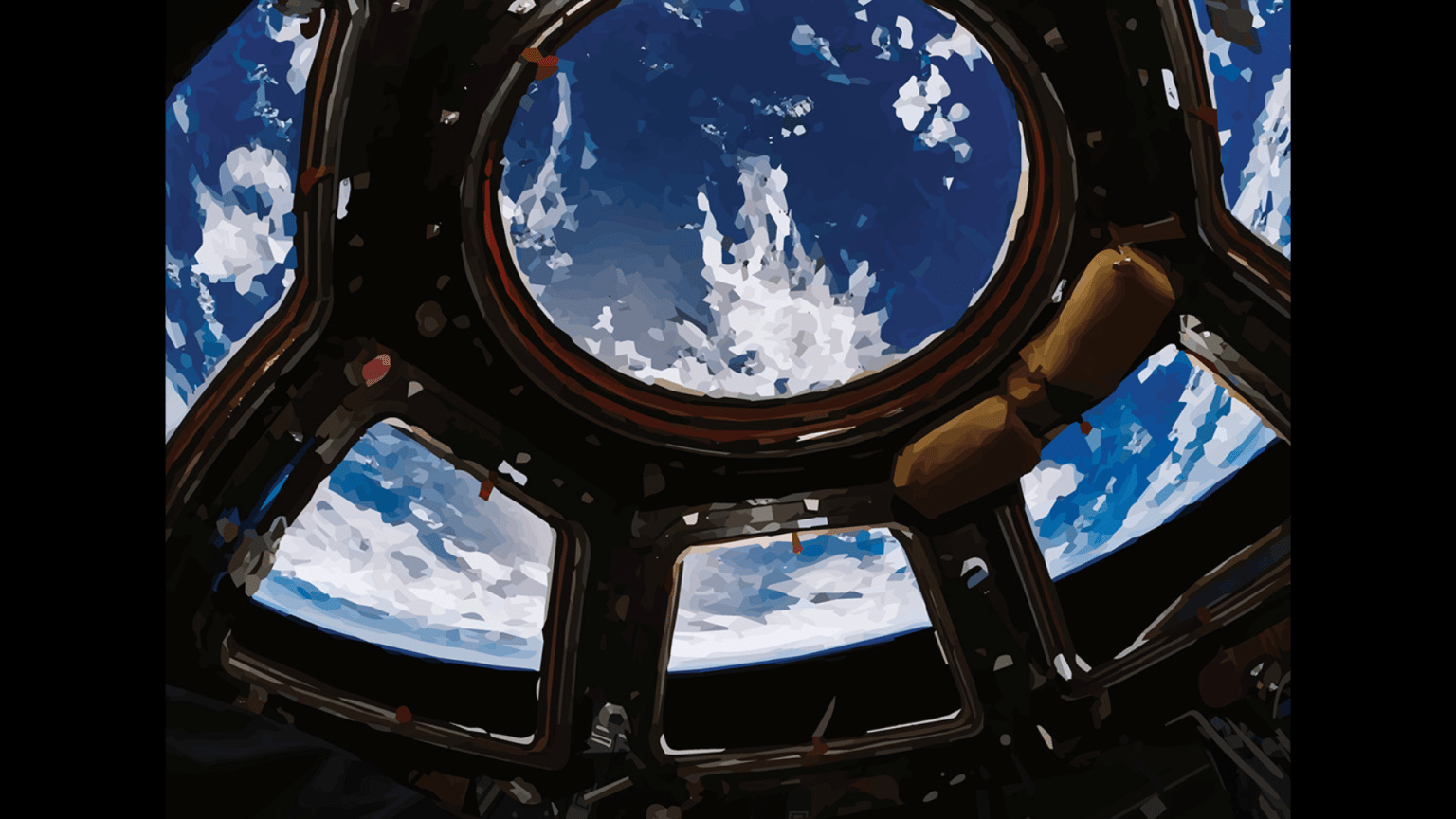
Tissue chips are small devices containing living cells that mimic complex functions of specific human tissues and organs. In microgravity, cells assemble differently than they do in laboratories on Earth and behave more like they do when inside the body. That makes the space station a unique platform for studies using these devices. Tissue chips also make up an important aspect of tissue engineering, which uses a combination of living cells and other materials to restore, maintain, improve, or replace biological tissues.
Cardinal Heart confirmed that microgravity caused changes to the EHTs. The next step, explains principal investigator Joseph Wu, director of Stanford Cardiovascular Institute, is testing whether certain drugs can prevent these altered effects during spaceflight and, eventually, help people with problems such as cardiac atrophy on Earth.
Using tissue chips to test the effect of drugs could help reduce the need for the animal studies that precede clinical trials in humans, currently the standard for approval of new drugs. Despite favorable results in pre-clinical animal studies, about 30% of medications are found to be toxic in human clinical trials and some 60% do not have the intended effect on humans.
“Tissue chips test potential drug candidates for human response and toxicity in a way that is more predictable,” says Siobhan Malany, principal investigator for Human Muscle on a Chip, which tested the feasibility of using accelerated muscle weakness in space to study age-related muscle decline on Earth. “So many drugs fail because of a lack of human efficacy or because of toxicity. Tissue chip technology is really filling that gap from early discovery to the clinic. Because tissue chips are robust, three-dimensional, and micro-scale, we can send many of these experiments up for longer periods of time to observe long-term and chronic effects.”
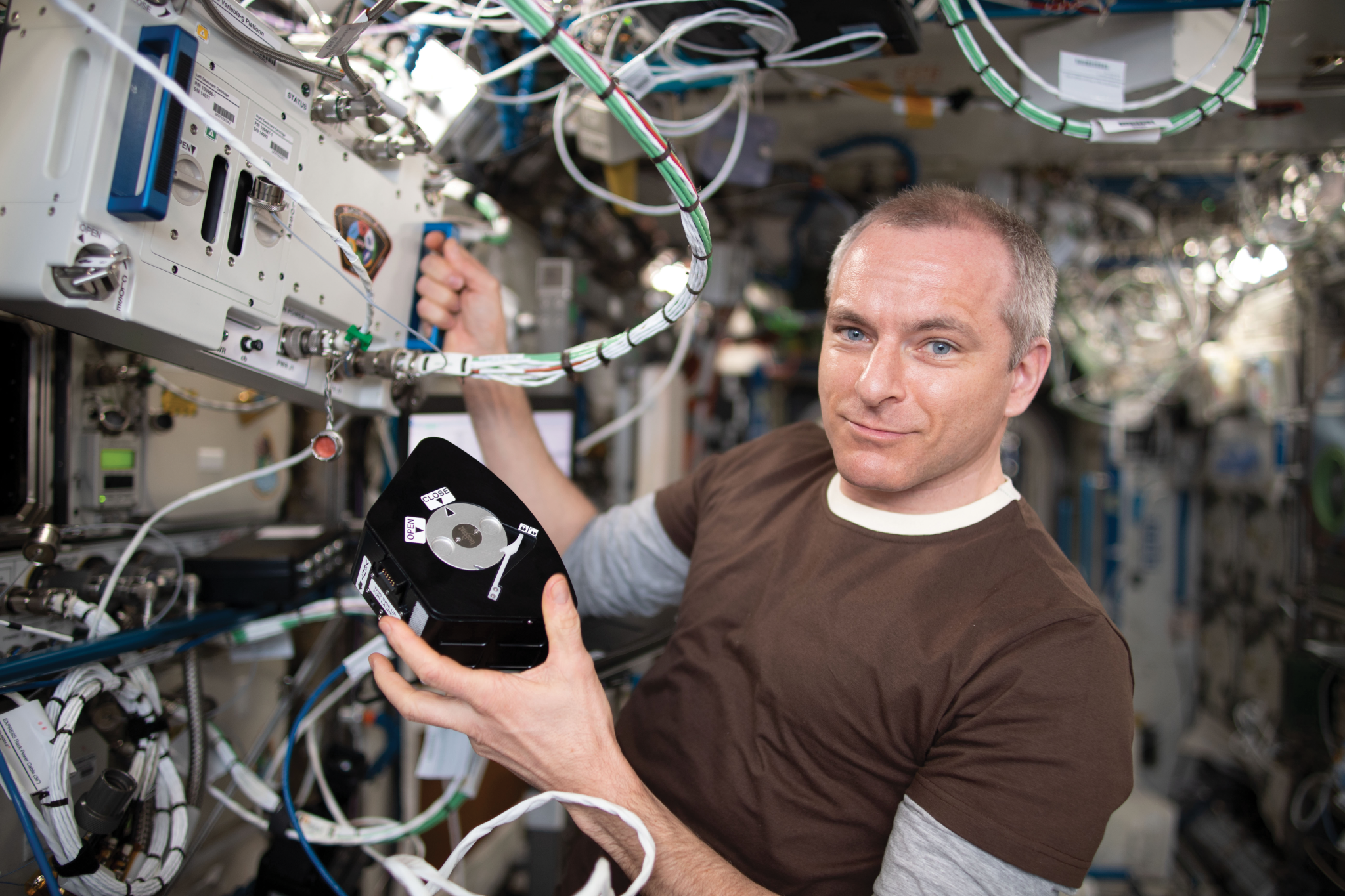
ESA (European Space Agency) developed its own experiment unit (EU) to culture cells in space. The SPHEROIDS investigation used EUs to examine the effects of microgravity on the function of endothelial cells. Endothelial cells line the inner surface of blood vessels and play a key role in vessel structure and regulation of blood pressure. Results published in the journal Biomaterials showed that endothelial cells formed 3D structures in the EUs with good viability for the 14-day test. The investigation also confirmed the functionality of the automatic medium exchange and fixation procedures. EUs could play a role like that of tissue chips in drug testing and research in pharmacology, toxicology, and radiation biology.
Malany plans a follow-up space station investigation to test whether a steroid derived from tomato plants, Tomatidine, improves muscle mass. “Basically, the same set of tissue chips will go back up to space. One gets the treatment and one does not, and we can look at specific responses and any toxicity,” she says.
A type of tissue chip with human knee cartilage developed for a study of post-traumatic osteoarthritis (PTOA) is helping advance development of drugs to treat the condition. PTOA can occur when traumatic joint injury leads to loss of cartilage and bone. It affects millions of people of all ages and is believed to be initiated by a “cytokine storm,” an over-response of the immune system following an impact injury such as a fall. International Space Station National Laboratory sponsored experiment MVP Cell-01 showed that low doses of dexamethasone, a potent anti-inflammatory, dramatically suppressed levels of cytokine in the knee following injury. A follow-up investigation combined the drug with a growth factor, and researchers plan to propose a clinical trial for the combination.
“Half of the drug development battle is discovery,” says principal investigator Alan Grodzinsky, a professor in the Department of Biological Engineering at Massachusetts Institute of Technology. “The other half is drug delivery: in this case, a technique to get a low dose of the drug into the cartilage. We can use this chip system to test delivering the drugs with nanoparticles. Using a real human system has many advantages over using animal ones for these studies. In the not-too-distant future, this work should lead to treatments for PTOA.”
Tissue chips provide faster results as well. “When you use a tissue chip platform, fabrication takes a few days,” says Dilip Thomas, a post-doctoral researcher in Wu’s lab at Stanford University. “Then, after you start treating it with drugs, depending on what measure you are looking at, you can have an entire set of data in one month.”
Tissue chip studies on the space station take advantage of the fact that many of the changes that microgravity causes in the human body resemble aging-related diseases on Earth but happen much faster. Researchers can model changes in days or weeks rather than months or years.
“Microgravity accelerates disease processes and also uncovers potential new targets for drugs. We can look at disease pathologies in a way that we can’t do here on Earth,” says Lucie Low, scientific program manager at the National Institutes of Health’s National Center for Advancing Translational Sciences (NCATS). NCATS partners with the ISS National Lab on the Tissue Chips in Space program, which funds these tissue chip studies. The program seeks to understand how microgravity affects human health and disease and to translate that understanding to improved human health on Earth.
STaARS BioScience-7 sent tissue chips to space to imitate aging of immune cells and confirmed that the cells age in microgravity and so provide a model for studying the process.
“We know the pathways involved, now we want to know whether we can prevent or even reverse the aging of immune system stem cells, which play a role in repairing our bodies and healing wounds,” says principal investigator Sonja Schrepfer, a professor at the University of California San Francisco. Even young people can have aged immune systems, for example if a latent virus continuously activates the immune system. Schrepfer plans a follow-up experiment that will bring tissue chips back from space without freezing them.
“We know they will be aged, and we will look at whether we can reverse that back in the lab so that stem cells behave normally and repair a wound or blood vessels at normal speed. The goal is to fully understand a molecule that we can eliminate or a pathway to block to prevent aging effects,” she says.
From the heart to the immune system, muscles, bones and more, these tiny stand-ins for human tissues are bringing about big results.