If you’re fascinated by the idea of humans traveling through space and curious about how that all works, you’ve come to the right place.
“Houston We Have a Podcast” is the official podcast of the NASA Johnson Space Center from Houston, Texas, home for NASA’s astronauts and Mission Control Center. Listen to the brightest minds of America’s space agency – astronauts, engineers, scientists and program leaders – discuss exciting topics in engineering, science and technology, sharing their personal stories and expertise on every aspect of human spaceflight. Learn more about how the work being done will help send humans forward to the Moon and on to Mars in the Artemis program.
Episode 123 features Dr. Jenn Fogarty who gives an overview of the Human Research Program at NASA’s Johnson Space Center. This is the first in a series of six episodes that dive deep into the work being done to understand what exactly happens to the human body in space. This episode was recorded on November 18th, 2019.

Transcript
Gary Jordan (Host): Houston we have a podcast. Welcome to the official podcast of the NASA Johnson Space Center, Episode 123, “Humans in Space.” I’m Gary Jordan. I’ll be your host today. On this podcast, we bring in the experts, scientists, engineers and astronauts, all to let you know what’s going on in the world of human spaceflight. Human spaceflight, we talk about it a lot. But that human element in front is a very important piece of the puzzle. It can make traveling through space a lot more complicated, what with redundant systems, that pesky little thing called life support and that heightened element of risk. But, in the end, a human can lean on curiosity and discovery in space exploration to do so much more, and best of all can share the experience that many of us can only dream of. A lot of work at NASA goes into understanding the human element in human spaceflight. In fact, there’s a program right here at the Johnson Space Center that focuses on just that. It’s called the Human Research Program. Longtime listeners may recognize this program from many of the episodes we’ve done in the past, namely, the series on the “Five Hazards of Human Spaceflight“, Episodes 56 through 61, for those interested. But there’s a lot more to the program, and it can be organized into different elements or areas of focus. So for these next six episodes, we’re going to dive deep into the work being done to understand what exactly happens to the human body in space, because there’s so much more work that goes behind that than you might think. Physiology, how humans interact with machines. Human behavior. It involves analogs on the ground or like pretend spaceflight in a sense, like habitats. It also involves other NASA centers, universities and international organizations. And all of this work helps us to be successful in space. It informs us now on the International Space Station and informs us on what we can expect on the Moon for NASA’s Artemis Program and for traveling to Mars. And it shows us what we can learn that can be shared and pulled into other areas other than human spaceflight for the benefit of humankind. So here to give us an overview on everything Human Research Program is Dr. Jenn Fogarty. She’s the chief scientist of the program, and today she describes the history of human research, the disciplines within the programs and why we’re focusing on these particular elements. So here we go, the history and elements of human research at NASA with Dr. Jenn Fogarty. Enjoy.
[ Music ]
Host: Jenn Fogarty, thanks so much for coming on the podcast today.
Jennifer Fogarty: Well, thanks for having me. It’s a pleasure to be here.
Host: We talk a lot about human spaceflight, and today, we’re going to talk about that very first word, human. It’s a very big part of it, and there’s a lot that goes into it, so we’re really going to have you break it down, and I’m excited for you to do that for us.
Jennifer Fogarty: Yeah, my pleasure. I mean that’s what I do for a living, so I’m always excited to talk about it.
Host: Yeah, you have a long history in human research. Let’s go through your biography. Tell me how this all came about for your career.
Jennifer Fogarty: Yeah, it was a bit of a winding road. I’m really glad where I ended up, and when I talk to young people today, I kind of give them the perspective that anything is possible, you know. It’s taking on challenges and opportunities and keeping your mind open along the way. So, I’ve always been interested in medicine and human health and how people stay well and how people get sick and how we fix them. That was, my earliest memories as a kid I was never shy of injuries or blood or anything. I was just deep into those things. [Laughter] I had three brothers, so there was plenty of blood and guts and stuff to see. [Laughter]
Host: Oh right.
Jennifer Fogarty: So yeah, it was, that was my passion from, just don’t even have a memory of it, just felt very intrinsic. So, always thought any kind of education that expanded on that. So, when it came time to make decisions about college, premed was definitely the track of choice. But then really understanding what premed was and kind of, you know, the reality of finances and how was I going to get there and do all these things. And I was actually first-generation college. My parents were children of immigrants, and so kind of how you face learning how to do these things and accomplish these tasks. So, didn’t get a whole lot of guidance, you know, and I think some of this takes a lot of support to overcome these things. A lot of different people manage. But anyway, it’s a kind of winding road. So I did biology as undergrad with a minor in chemistry. I did really well in college. I was, really liked being a student, loved to read, so getting grades wasn’t hard. But applying it is the key. And then it comes to the decision about graduate school. Where are you going to go, what are you going to do? And when I was struggling a little bit and kind of, you know, each kid is trying to stretch their wings and figure out what to do, I decided, I’m from New Jersey, I decided to leave and kind of came west, all the way to Texas.
Host: Alright. [Laughter]
Jennifer Fogarty: Ended up applying, getting accepted to Texas A&M College of Medicine, but to the PhD program. So I really was fascinated with the research side, how medicine becomes medicine. Like how do we know to do the things we know? How do those things, how do new treatments come about? Where do they come from, and how do we understand the human body? So I spent five years up there working in a Department of Cardiovascular Physiology, Medical Physiology. Completed my degree, and this is really where the turning point was of space. I was aware of it and really understood aerospace medicine because two of my brothers are in the Air Force. My parents worked for the (Federal Aviation Administration) FAA, so I understood like aviation, general aviation and things like that and understood kind of hypoxia and when people went to altitude. That was kind of a common discussion across the dinner table about pulling G’s and what are called G-LOC, which is gravity induced loss of consciousness, so when fighter pilots pull really high G’s. You can’t even feel them in your car like when you take a steep turn at a high rate of speed, something pulling you. They can take up to eight G’s, you know, pulling different maneuvers. And they learn how to stress and strain against it, and they wear a protective suit. So, understanding those kinds of stressors on the human and how you survive them. So along the way, I was doing my work in a lab by a gentleman named Dr. [Michael] Delp, and Dr. Delp got funding from NASA for an experiment and was actually on Columbia-107. So my first experience was getting ready, because we had a certain technique we did. It wasn’t the same work I did from a study perspective. But the way you prepare these vessels and study the cardiovascular system was something I specialized in and was good at. So, he said do you want to come with me over to Kennedy and work on this program? And I said sure, I’d love to take a couple months and go do that. So, we moved essentially his entire lab over to Kennedy Space Center, and of course, we’re prepared for our experiments when the animals returned on 107, but unfortunately, 107 was one of the vehicles that did not return.
Host: Right, the Columbia accident.
Jennifer Fogarty: The Columbia accident. So, I spent a couple of months out there, because one of the things that happens was they lead sealed the doors for all the labs, so all the equipment was locked in. So a bunch of people had to go back to Texas A&M and kind of resume their lives. But because I was in a postdoc position, I had some latitude. So I stayed there and just started reading and learning more about NASA and kind of maybe there was a place for me there. So I started looking for jobs, and about six months later I applied and got a job with a local contractor. At the time it was Wyle, now it’s KBR Life Sciences. And started working in medical risk management on the cardiovascular side supporting space medicine. So, that was kind of my entre into NASA.
Host: What a career path. You were already at NASA when you were thinking huh, maybe I should pursue something. You were doing research at the Cape, right?
Jennifer Fogarty: Well yeah. And for me, it was, you know, maybe knowing how NASA kind of has work at different centers at that point, becoming familiar because the grant came from a program that was out of Ames Research Center. I thought well maybe that’s where, you know, my skillset would work best. But one of the opportunities came up, and clearly I was only two and a half hours up the road at Texas A&M that I came down and interviewed and luckily enough got to work at Johnson Space Center, which is the manned spaceflight center. And my work that I did for my dissertation was very human relevant. It was on cardiovascular disease and people and how to get past those blockages in your arteries and build new vessels. So, I had a lot of background in doing medically applicable research. And that really was beneficial to space medicine at the time. So I worked with the flight surgeons and with the Chief Medical Officer on kind of selection standards and kind of when medical risks came up and people were being treated, what did that mean to the mission profile? So I spent about 12 years working in the medical side of operations and also worked for what’s called the Health and Medical Technical Authority.
Host: So, with your background in how the cardiovascular system works in the human body, what was particularly interesting? What questions were you looking into when you were just starting to get into this world of human spaceflight?
Jennifer Fogarty: Well the one where I kind of, my skillset really played into was a thing called orthostatic intolerance. So it was happening, you know, when crew members return, this goes all the way back actually to Apollo, not quite Mercury and Gemini, and we try to understand why those, why that is true? But the longer you spend in space, your body does a really good job at adapting to it, right. And it’s not, and I’ll probably expand upon this again more later, because it’s super interesting and I think is a little bit of a different take than what people have heard before about spaceflight. But this adaptation is not only perfectly normal but perfectly appropriate. Where it creates a challenge is when you want to change environments very quickly. So when you want to go from microgravity and being in space to coming back to Earth on the order of hours after being in one of those domains for a long period of time, your body is going to have to do another adaptation. And sometimes the amount of time it takes you to adjust is what makes understanding what does the vehicle have to provide the person? What is the person capable of? That space where we have to do research to be able to describe how do you keep that person safe and healthy while their body is readapting. So, again, kind of Apollo, Skylab, definitely during shuttle is where we saw a lot of examples. When people come back to Earth after being in space for a while, and then they go to stand up, there’s a couple of things going on. Definitely your neurovestibular system, that organ in the middle ear makes you a little dizzy, so you got to learn where up is again and understand what gravity is to you. But the other thing is your blood vessels actually decided to maybe not do their job the same way in your lower body, and that blood that should be coming up to your head and heart and your lungs kind of sinks down to your lower body and fills your legs. And it’s really hard to get it pumped back up. So it causes this thing called orthostatic intolerance where it, when you stand up, your heart rate will get really high. Your blood pressure starts to drop. And eventually, if unsupported or if you don’t do something about it, you pass out. Yeah. So.
Host: The same thing happens to me in the gym when I try to do squats.
Jennifer Fogarty: Yeah, exactly, and for the same reason. You are collecting a bunch of blood in your lower body where you have a bunch of big muscles, and it’s no longer accessible to the upper part of your body. So that’s why when you stand up out of a squat, like your eyes, you kind of get that tunnel vision, and you know like oh, if I don’t do something, I’m going down. [Laughter] So you need to start walking. It’s called a muscle pump. So you use your own muscles to push against your blood vessels to push that blood back up to your heart, which gets it to your head, your brain. So it’s the way your body’s actually designed to manage the fact that if you’re not getting good blood flow to your brain when you’re upright, your body lays itself horizontal where there’s no gradient, where your heart doesn’t have to work very hard to get it from one side to the other because it’s all in the same plane. The issue is why it’s happening? So, what you’re describing with a squat is pretty normal, and you know to move. The other thing is dehydration could be factored into it if you’re working out really hard. You need more volume. You need more plasma volume. You need to get water into your system and into your blood supply. But really, it’s about sequestering that blood, hiding it more or less in your muscles. And sometimes it actually goes out of the muscles and the blood vessels into the tissue, and that’s called third spacing. And the only way to get that, you can’t get that volume back into your blood supply. That comes out through what’s called your lymphatics. And it’ll be made into urine and it’s kind of lost. So, when crew members came back and they discovered that a couple of them they were, again, you’re measuring blood pressure. You’re measuring heart rate. You see these signs tell you that the orthostatic, you know, they’re not going to do well on their own, right. Or they need a garment, as I mentioned before with the high-performance jet pilots, an external force. So instead of you walking, like if you don’t have the ability to, because it might be a small volume or you don’t have any place to walk to, if your muscles can’t contract, this suit presses on you. So G-suits fill up. They’re usually air bladders, and you can crank up the pressure using a dial to say how much millimeters of mercury pressure do I want to apply to those muscles which also applies to the blood vessels to keep that column of blood going up to your head and heart. So, we actually have used G-suits on the crew members since the Apollo era, because it was a well-known Air Force solution to having a hydrostatic gradient that was pulling blood away from the head and the heart. The issue is that it’s meant really for you not to be walking around. They’re not usually designed to be ambulatory. They’re meant to be seated, which is what a pilot is. So we’ve had trouble translating them to something that really works for walking. Now the Russians have a solution which is called the Kentavr, and it’s a very practical solution. So you have fabric that has lacing down the side. And you can imagine they’re like a pair of bike shorts that come up along your hips up to your waist. And then there’s also a segment that’s on your calves. And you can customize the tightness by how tight you lace them. So it’s just a real practical solution.
Host: Squeezing the fluids upwards.
Jennifer Fogarty: Yeah, so it’s going to keep that column of blood, it won’t allow it to expand. It’s really hard to tie them tight enough that you get active contraction. But it’s just not going to allow it to come out more. So it’s an external support, like a girdle type effect. And it’s been very successful. And we actually, our crew members use them when we fly on the Soyuz capsule. And we’ve done experiments with them to understand could we quantify how well they work? The nicest part about them is that they are customizable at the time you wear them. One of the changes that happens in crew members is it’s called chicken leg. So when they go into orbit, their lower body does get smaller. They have a little bit of muscle atrophy, but they actually just lose a lot of blood volume out of their lower body. So, if you were only to measure and fit somebody for a G-suit before they left, it would be the wrong size when they returned. It would be too loose.
Host: Wow, there’s that much change.
Jennifer Fogarty: There’s that much change. It returns to like preflight within a week or so, but that doesn’t help you on landing.
Host: Yeah, you need it when you need it.
Jennifer Fogarty: You need it when you need it.
Host: What I’m hearing, what your describing, you know, when it comes to what’s happening to the human body in space is these extreme environments put a lot of stress on the human body. The human body adapts, but there’s a lot of changes. And so a lot of work at NASA and other places, when it comes to human spaceflight is developing technologies to maybe help mitigate some of these issues, and that may be just one example. But really, it’s trying to identify what exactly is happening. And it seems like we’re still looking into that.
Jennifer Fogarty: That’s right, it’s been an endeavor to characterize, because the other complexity is people respond so differently, right. When you think about the uniqueness of each individual, what state, how they start, how much change occurs, in what direction, in what system, so when you talk about the musculoskeletal system, talk about the cardiovascular system, talk about the central nervous system, talk about the GI system. So I talk a lot of times when I do give lectures, I call them dials. Like if you can imagine each one of those systems being a dial across, you know, a table where you’ve got to control them. Or you watch them change. Then you’d say, OK, in what combination do I turn some of these dials so that that person has the best outcome. Like all those dials add up or potentially multiply together to equal the sum of its parts. And the whole is actually, as stated, typically greater than the sum of its parts, right. You can just try to measure each one very isolated and think you can add them up and get the answer and guess what, biology fools you every time. [Laughter]
Host: Wouldn’t it be nice if there was one solution to fit all, but that’s not the way humans work.
Jennifer Fogarty: Right, so a lot of our work ends up going across many humans. So you hear a lot about, especially with, you know, the recent [Extravehicular Activity] EVA was two women. It was, well how different are women? Are we making sure we understand across both sexes, across multiple heritages and races and, you know, backgrounds of any sort that you can imagine that influence, you know, lifestyle factors, that would change potentially outcomes. And also, the experience base that you come in with. So you talk about working out at the gym. So we have, you know, requirements for people to be healthy, of course. You know, you think about the astronauts and their robust human beings that are intelligent people that dedicate themselves to this endeavor. So, they are very invested in their health and wellbeing, so they take an active role in being very healthy individuals. But even when you work out, you could be squatting the same as another person and have very different outcomes. You’re like why do I put on muscle, but this person doesn’t? And how come I can’t get rid of that body fat?
Host: The story of my life, really, in the gym. [Laughter]
Jennifer Fogarty: Pretty much. And then you see how complicated it is when you add on dietary factors, right, where, you know, supplements or, you know, you hear different fad diets that come up about and say one works for one person and one doesn’t for another. Like, what is causing the difference between these people? And that’s when you get into omics, you know, whether it be genomics or epigenetics or protium, the omics go on and on and on right now. But it’s really understanding someone at a very molecular level to know if that is a key to understanding what’s the better outcome. So, in addition to all the work that we do that characterizes the biology and the physiology, we’re also moving into the domain of characterizing people on a molecular level. And you kind of have to think of it as a puzzle, that you don’t have the picture in front of you. You have a lot of pieces, and you don’t have the edges. So every time we get a piece of information that’s about characterizing or measuring something you say OK, do these pieces link together? Do they relate to each other? And do they affect a dial? So it’s, for me as a chief scientist, it’s really looking at everybody who works for NASA, who’s funded by NASA and actually, we even go beyond that because we rely on terrestrial research who are studying humans to give us clues about just humans. Because a lot of what we do is yes, you mention space has a lot of stressors and a lot of, those, pardon me, those are challenges, right. And even in the case of exercise, you intentionally go and stress your body, right. That’s when we perceive stress to be a positive event. And so there are a lot of conditions where your body is responding to that stress. And the next time the reason you build muscle was because you broke it down. You caused a little bit of damage, and your body said all right, I’m going to repair myself and put a little extra down because the next time you come back and do that, I want to be prepared for it. And that’s actually how you lay muscle fiber and get stronger and larger. And if you keep on adding load and keep on adding reps or do different types of intensity, you change the stressor, so your body has to continue to respond. So in our case, you have people who have done that for their lives going into spaceflight, and now in some ways, we take away stress. So going into microgravity is removing a signal. And so now the body’s trying to consider, well do I continue to invest in this thing when you load me? Your bones and muscles in particular. Or do I kind of pull back on that investment because my energy is spent better elsewhere? And so the other kind of throw down term I use sometimes is the energy, the human body is the most energy efficient machine known to man. It will stop investing in things if you stop demanding of it. And when you demand of it, it’ll go put energy in over here. And sometimes that makes a process we’re not very fond of, you know. In our lifestyles you hear on Earth like with the rate of cardiovascular disease, you’re like well why is that? You know, where is that coming from? What are we exposing ourselves to or what are, why are we inducing that process? And you know, you look down at this point they were like well, we look at a lot of the foods we eat and the types of foods we eat and the things that are in the foods we eat. But how does your liver respond? What have we set off in your liver which makes the lipids that aren’t so good for your blood vessels, why is your liver responding that way? So, it’s understanding cause and effect between a stressor and a response and then saying is that somewhere where we need to interfere or is there a different location that makes sense to kind of interfere with a process? So in spaceflight, when people say oh, you know, we want to stop bone loss and we want to stop muscle loss and we want to stop, you’re like I understand where that comes from. But, you know, that resistance to change, thinking that’s how we keep them healthy. But in all honesty, you’ve got to allow, you’ve got to be willing to think that change is not all bad. It’s about does the change allow the person to accomplish the task they need to accomplish? So are they strong enough to do the job when they get where they need to go? So in the concept of us doing Mars exploration, after spending six to nine months in transit, probably in microgravity like they are today on the space station, you’re going to see changes. Do we have them in a position on the day they land on Mars to be healthy and well enough to take care of themselves, recover, because it’s going to be a rough landing, they’re going to have to transition, but then are they strong enough to deal with what’s 3/8’s gravity, 3/8’s of Earth’s gravity? Will they be strong enough and healthy enough? So then we talk about, you know, risk for injury, whether it be fracture or, you know, muscle injuries, if they need to go off and do work. So we say, how do we measure change over time? And then how does that change match to the expectation and the outcome at the end? Which is for us is being healthy and well to live and work on Mars for some unknown period of time. OK, now we haven’t quite gotten that data yet.
Host: That’s right. So what I’m hearing is there’s a lot of different fields, a lot of different considerations when it comes to human research. I’m hearing a little bit of overlap too between human research in space and human research on the ground and how this can be applied to even our own lives. So, I wanted to take kind of a step back and go through the history of Human Research Program and what we’ve been doing at NASA that’s led up to this point and how it’s organized now, to tackle all of these problems and all of these different areas that you started with. Let’s go back in history. Let’s take a look at human research through the beginning of when we started looking at it and the early times of NASA.
Jennifer Fogarty: Yeah, and even, you know, the 50s, 50, 60 years ago, when you talk about the program that was in place, it was mainly medical to support the astronauts, whether it be Gemini, Mercury, Apollo, there were lots of unknowns. It was a very scary time. There were lots of hypotheses about what may or may not happen. It was really Mercury and Gemini that set the stage for when you put someone, and even the Russian attempts at same, just survival, you know. There were questions about could people swallow in microgravity? Thinking about, because the concept was, and not different than we think of it today, was you know, being almost upside down.
Host: Yeah.
Jennifer Fogarty: Right. Could you swallow against a pressure gradient or force that was in a different direction or lack of force. You know, it was just very confusing, and we didn’t have a good way to simulate it. So the people who went before us had a lot of unknowns. You couldn’t have told them what to expect. Really, it was about them telling you what they experienced. There were some animals sent ahead. You hear about the famous dogs and, you know, monkeys that went and survived. They ultimately may not have but not because of microgravity. You know, there were other problems with the vehicle or the way it came back. But I would say the premiere medical side and the data that was collected during Apollo where they did biomedical monitoring really set the stage for like well what was your blood pressure doing? What was your heart rate doing? What was your body temperature doing? And when did it change and why? And a lot of it had to do with psychological stress. I mean you talk about the Moon landing itself and kind of just suggesting, so the first time that lander was coming down, and they talk about the heart rates, you know. It just told us a lot about well it was a very normal response to something that was pretty scary at the time, right. Very low fuel. They were getting callouts about how close they were to the ground and having to put that lander down.
Host: This was the Apollo 11 landing, right?
Jennifer Fogarty: Yeah, Apollo 11, yeah. So when you hear that audio recording, you yourself as a listener could get high heart rate, right. You can feel the stress and pressure that was going on. But we started to learn a lot about what happened that was completely normal. People were able to eat. People were able to sleep. The questions were, did we make it comfortable for them? Did we make it reasonable for them to live and work in that environment? Or did we cause more stressor than just being in space? And that’s part of the work we do now so we don’t add extra stress. But as that evolved from that Apollo biomedical program, the agency started to formulate something that was a little bit more structured which was called the bioastronautics roadmap. And through Skylab, which was actually a dedicated life science mission, and the biomedical results of Skylab which are several books on, you really start to learn about people being in space for longer periods of time and dedicated study of the human body. They even flew physicians for that purpose. And they went up in incrementally longer missions over the three Skylabs, so it was 30 to 60 to 90 days ultimately that they spent in space. They tried different modalities of exercise to see how that would work. And interestingly enough, all the Skylab crew members either maintained or gained weight. And they were more fit based on the exercise testing when they came back than before they left.
Host: Wow.
Jennifer Fogarty: So when you think about the human ability to respond and rise to the challenge, if you give the body a challenge, it will respond. Microgravity was not an impediment to that. But, now it was about understanding, as missions changed and vehicles changed and the mission of those vehicles changed, if you’re not dedicated for studying the human body and just working on it full time, maybe you’re going to have some changes that are not negative, but you’re going to have a decrease in body weight or a decrease in muscle mass. And it wasn’t because the body couldn’t do the opposite. It was just that we didn’t provide the stressor because you’re competing interests. Moving into the shuttle era, you know, those missions were about 14 days or less. We had several that were called extended duration orbiters. And one of them was, more than one of them was Extended Duration Orbital Medical Project, EDOMP. And there’s actually several books on that that talk about all of the biomedical research that was done on shuttle. But again, shuttle, the way we talk about it is like a sprint. A two-week mission, maybe 17-day missions, but packed full of operations. A lot of it was science at the time, but a lot of it was construction. It could have been launching satellites. It could have been fixing telescopes, constructing the International Space Station. So when you are working full time, eating and exercising take a back seat, just like in your everyday life. So we started seeing people lose weight, and their body composition change a little bit, even in a two-week period, and we could measure it. And that’s really when we started discovering things like the orthostatic intolerance. Because we had a lot more people flying. We had men and women flying. And they were dedicated toward operations. And so the human need kind of took a little bit of a back seat. So, that led to a lot of understanding about what we were capable of doing, depending on how you designed the operations of the mission. In 2000, when they launched space station, the idea was these people were going up and going up for longer durations. At the time it was probably more like four months, three, four months, not quite the six months and more that we’re doing now. But that’s a marathon compared to shuttle. And so you really had to understand where were we going with expectations on the human, and were we providing what the human needed over time to still be healthy and functionally, perform well, given that they had a mission to do. And even during shuttle, I came to NASA in 2004, so early part of ISS, the evolution I’ve seen in the International Space Station, finishing construction now in its utilization phase, but also how we think of managing the crew and their health and wellbeing both physically and psychologically over time is to sustain them over very long what is essentially deployments. So, it’s evolved the way we do our science, the way we’re trying to study the human plus the techniques have become more and more modernized as terrestrial techniques have, of course. But it’s with that eye on exploration because we’re using that platform, ISS as Mars forward. So you say if you do 600, which is why we’re asking for a year on station like we did with Scott Kelly and Mikhail Kornienko. Because time course, understanding the change over time, is incredibly important for us to be able to predict other time courses. Because we’re really being asked for mission to Mars being anywhere from 24 to 36 months, depending how long they actually stay on the Martian surface. And those are just really unprecedented durations and exposures. So, if we want to have any confidence in what we’re predicting, we need experience and really some solid data throughout the mission, and I’ll expand on that a little bit, than we did before. Because the most robust measures you can do are really pre-post when we get them back on Earth, you know and you think about big machines like (Magnetic Resonance Imaging) MRI, invasive procedures where they’re a little bit more risky to the person you want to make sure you want to have a sterile environment. So on space station, or in any, even on shuttle, we tend to do things that are very minimal, very, as much noninvasive as possible to keep the risk down to the person to the mission. But you really struggle for good what’s called time force data from a science perspective. So we’re trying to fill in those gaps in the middle and not just rely on pre-post. We need a lot more data in the middle.
Host: Data is good.
Jennifer Fogarty: Data is good.
Host: That’s why we have the space station is a great place for that. A lot of people going up, so a lot of datasets. You mentioned 2004 was when you came to NASA. I think that was about the same time HRP started, the Human Research Program. So, you mentioned you’ve seen a fundamental shift in the way that we approach long duration spaceflight and the priorities of people in space. Tell me how that’s progressed from when you came on, with maybe specifically the Human Research Program but really, really focusing on that progression. What were the questions we were asking and then filling in the gaps for?
Jennifer Fogarty: Yeah, so it was a real, I think, fortunate time because I saw both sides of it even though it was the tail end of what was called the bioastronautics roadmap. So you’re right, it was about 2004, and that had a lot to do with the development of Constellation and how the agency was reorganizing itself to support Constellation which was, of course, Orion and SLS at the time and a bit of a different structure. So, the concept was with bioastronautics roadmap that the mandate was every broad. It was a lot about doing excellent science, excellent study of the human, but it didn’t quite have the mandate to be very mission-oriented with the concept of a Mars mission only. It was a little more open than that. So, it didn’t have that applied mandate. And with the formation of Constellation, the restructure with kind of in the agency, there was a shift toward needing a more dedicated applied human research program. So, they did actually stand up in around 2004, 2005, we did a lot of work to develop the content and kind of down select what needed to be focused on, which resulted in kind of the risks you see today are articulated in the Human Research Program and the human research roadmap. But it was quite a process through a lot of boards, a lot of vetting, a lot of external oversight of how those decisions were made, different priorities. But it did ultimately kind of segue itself into the Human Research Program. And the elements that you see today, I think we’ve done some collapsing because we understand the integrated nature of things. But it was broken out to kind of represent the five major disciplines that we thought existed at the time that could cover the content that would lead toward more applied results so that our focus is producing results that actually translate into an operational impact. And as you mentioned before, it could be technology. It could be a way to monitor something. It’s definitely going to have to be the evidence base to interpret what you measure and then the idea of actionable. What came out of this, that means we take what action for the individual. And then on top of it, we’re also responsible for the medical architecture which says when you can measure something, you can interpret it, and you know what actions you take, you’d better have the medical system to do it. So what do you prepack? How do you send someone with a medical system when they do need care, and you can document that, how do you make sure the care is there for them to have? Because you already had to know that ahead of time.
Host: Yeah, there’s a lot of, the way you’re saying this is structured, there’s a lot of practicality, there’s a lot of preparedness versus maybe the idealistic approach where, you know, you have to fit it into operations. So how can we best make that efficient?
Jennifer Fogarty: Yeah, that’s exactly right.
Host: So let’s go into how, you just talked about five elements that makes up, what are the five focus areas of Human Research Program?
Jennifer Fogarty: OK, so right now we have human factors and behavioral performance. And that actually is one that is a collapsed group from the early start of the Human Research Program. So, and there’s a lot of overlap when you think about the psychological underpinnings of how someone is managing their environment and their wellbeing in an environment. So when you think about where you live and work here on Earth, you’ve got a lot of latitude to probably change your environment. So you could reorganize your office. You can reorganize your home. You can add and subtract furniture. If, you know, in certain cases, if you’re dissatisfied with your location, particularly your home, you can go buy a new one. Your office, not so much. But you make do. But you’ve got some freedom to alter your space, to suit yourself. And if you don’t, you actually have some recourse to probably go make something else happen. In the case of spaceflight, once that vehicle is designed and those decisions are made, pretty much there’s no latitude to make a lot of changes and accommodations.
Host: You’re stuck with it.
Jennifer Fogarty: Of any real significance.
Host: Sure.
Jennifer Fogarty: You’re like yes, you can put different things up on the wall and you might be able to move some stuff slightly, but in general, it is a fixed location, and it’s definitely a fixed volume. And the volumes you’re talking about are incredibly small. Station actually right now is a very large volume with respect to what we think the future exploration volumes will be. So we make sure people understand that it is a national laboratory dedicated for science, but it’s not as isolated or confined as one may think. But having said that, the human factor’s behavioral performance also studies the psychological health and wellbeing, the emotional health, the psychosocial health, because the idea is I mentioned before the word deployment in the Department of Defense and military deployments, we very much recognize the stressors that go along with being far away from family, having limited communication. Understanding the trials and tribulations are going on back at home and you can’t help, you know, those feelings. And your family feeling like I don’t have access to you. You’re not there for me. Well, for astronauts, it’s very much the same paradigm. So we can learn a lot from each other in that arena, but we have different circumstances in that we can’t bring somebody back from deployment very easily, especially on exploration missions. It’s actually not an option at all. Once they burn for Mars, they will have to go to Mars to return. So there’s no option of terminating that mission early.
Host: That’s just physics.
Jennifer Fogarty: That’s just physics.
Host: Yeah.
Jennifer Fogarty: But preparing someone and the family for those expectations and knowing how to handle them and the idea of communication will become harder and harder. That communication delay is only going to grow and make it impossible to have a real time conversation. So how do you manage the psychological health of someone when they’re going through that process? What tools do they need to manage that? And what kind of avenues can we give them that, like we called them before, countermeasures, relief, so that they have some connection back to home. Because even in the most extreme case, not only are they going to lose communication, but they will lose sight of the planet Earth.
Host: Yeah, that’s right.
Jennifer Fogarty: And there’s lots of concerns about that eventuality.
Host: It’s starting to make sense why these are intertwined, right. The human and machine integration but also that psychology, you know, that mental state of being in space and being in this spacecraft. You can see why those are intertwined.
Jennifer Fogarty: Yeah, because the vehicle is going to have to compensate in a lot of ways. So when we talk about some of the countermeasures being augmented reality or virtual reality, well those are all great ideas, and we test them. And there’s a lot going on here on Earth, you know, particularly in the entertainment community, about what those things bring to the table and how you use them. There’s a lot going on with training people with them, immersing you in an environment before you actually go there. So you have a different level of experience and training. But we have to go as far as writing requirements that tell vehicle designers what that means to have them on board. You know, not even from a physical manifestation. That’s one element. But how do you move data? How do you give it proper power? How do you make it available for four people or six people or whatever the number is going to be? Those are very specific needs that we have to articulate, because if we don’t do that, it’s not just going to be there by accident. It has to be there very intentionally and by design. So the level of detail we have to come up with to express to the designers and the planners what that means. And then the operational use of it. You know, when does it most benefit them? How do they get access to it? So, those are very much intertwined. I think it’s working quite well. That’s one of the elements, and I’m going to deep dive into those. Extraordinary work going on for sure. We work in a lot of different venues to try to really tease out some of the different stressors. So some interesting work in Antarctica and Moscow and actually here at Johnson Space Center. So, we don’t turn down an opportunity to study exploration and isolation for sure.
Host: For our listeners, stay tuned, because we are going to take a deep dive into each of these elements. I think the next one is, the one I have at least on my sheet is exploration medical capability.
Jennifer Fogarty: Yeah, so before we talked a little bit about that medical system of the future, those are the folks that are responsible for understanding of all the data coming out of our program, out of terrestrial medicine, pretty much any way where we can get it. Like, how do we envision the medical system of the future? Because right now, most of the time as people receive medicine, it’s a very personal and in-person experience, right. You go to a doctor, at a minimum, you talk on the phone. But normally, you go physically to the office to interface with someone or physically to a hospital. Remotely and on space station we have things such as telemedicine. So we use a lot of devices such as ultrasound that can take images. We’ve got video where we can look at crew members and watch them do a procedure. We can talk to them about their symptoms. You can get a sense of the color of their skin and, you know, how do their eyes look. And you can have one crew member examine the other crew member to give us that kind of physical report. And telemedicine can work really well. Because a lot of that data comes down and will go to the specialist to interpret and provide care. In the future, because of the communication delay, telemedicine won’t work. It’s just not practical. There’s no way to communicate. You’re talking in the best case scenario in the Mars orbit, it’s 20 minutes each way for a piece of information to move. So 40 minutes roundtrip to communicate a word or two or a sentence back and forth that’s typed, not spoken. In some cases, depending where the orbits are, the sun could completely block us and for many weeks to months we could have total blackout of comm. So, and there are some different strategies saying maybe you could get around that, but it’s not going to be less than 40 minutes. It’s going to be a lot more than 40 minutes to ping a signal off different satellites that are deployed. But the reality was telemedicine isn’t going to work. So how do we give, not only the physical tools to do medicine but the decision support? How do you give crew members, and one of them, you know, based on our standards and recommendations, will be a trained physician. But you can’t rule out that the physician won’t become ill.
Host: Oh yeah.
Jennifer Fogarty: You’re still going to need a lot of decision support, and what does that mean? So that’s often like, you know, people might go to WebMD or whatever to read up, you know, whatever research you can get on the web. But we want to create kind of the ultimate in a decision support tool that gives them the best evidence base. So when they enter symptoms or describe a problem that themselves or another crew member is having, it can bring up kind of a differential diagnosis that they can walk through so they can understand, well what test do I do next to narrow down what problem we’re having, and what is the ultimate treatment? It also has to be connected to the medical kit, the idea of well, if we’re going to give advice on what treatment, we should have that treatment with us. You know, suggesting taking something that you don’t have with you doesn’t do anybody any good. So we’re also going to have to have inventory management to understand what’s there. And there’s a lot of different solutions to this, I mean even potentially people want to talk about 3D printing of medications. And that’s all very good and synthesizing stuff real time is really very interesting. But that also uses a lot of resources, and you have to take a lot of raw materials. So, part of our job is to quantify the different options, test the different options, and that’s where we use station as a national lab say maybe to troubleshoot some things. But then explain, it’s called trade space if you’re going to take a band-aid or you’re going to take an ibuprofen or if you’re going to take a different medication, they all have to be compared to one another about how often would we use them, how much benefit to get from them? You know, how many outcomes does this impact, and how much do we have to take per person for the crew? So, the exploration medical capability folks ingest a lot of data. They also do a lot of modeling and probabilistic risk assessment, and those are data hungry tools that we just have to keep pouring more and more data into, and we have to partner with groups that are collecting data such as the (Food and Drug Administration) FDA and (National Institutes of Health) NIH and other entities that we might find that are interested in working with us. We do a lot at conferences to talk about who’s got data out there that can help us really sharpen kind of what does it mean to be a human and how do these decision support tools evolve. Because they’re actually more and more common even in hospitals and in the office space to give doctors kind of the real time feedback on, especially when they’re looking at something unusual and they have to do a, try to do a rapid diagnosis, there are definitely some decision support tools evolving out there. And even something like you hear a lot about IBM Watson.
Host: Right. Something smart, in-house, not connected to the internet.
Jennifer Fogarty: Yeah, and that’ll be our case in terms of we could in the background upload new and different stuff, and it would be vetted. That’s the other part of this that we don’t do anything that’s not validated. So it takes a lot of work to say we’re very confident and comfortable that this is actually the data that we think is really the data that should go and inform the crew versus a lot of folks they’ll say, well why don’t you do cutting edge, or you know, this is the newest journal article that came out. And I was like well that’s great. Now we got to see the test of time.
Host: Right.
Jennifer Fogarty: You know, it has to be redone. Someone else has to independently verify that those are accurate results before we would kind of really ingest them.
Host: Yeah, maybe reliability is more of a concern. But what it sounds like, what it really comes down to is deep space exploration has a lot of constraints. If you could, you could just bring everything you wanted and have instant communication, but that’s not the case.
Jennifer Fogarty: Yeah. And it comes down to, I mean when we say vehicle, I think it conjures up a car or a plane what people are used to and kind of the paradigm of being able to get more or different along the way. And for the Mars mission, that’s not the case whatsoever. You can’t even do resupply. You can pre-deploy and catch up to something. But you still had to prospectively determine what that stuff was you sent. So I always describe it now as, you know, we’re really building an exoplanet. We’re not really building a vehicle.
Host: Wow, that’s an interesting way to think of it.
Jennifer Fogarty: Because I think it kind of makes you step back and like, oh if I had to think about all the air, water, oxygen, food and nutrients, all the medical like, that’s a much bigger undertaking than the concept of a vehicle, to me anyway.
Host: Yeah, absolutely. Let’s go to the next one. The next one is countermeasures, human health countermeasures.
Jennifer Fogarty: Yeah, so this is really where the physiology, the deep dive into human physiology, that change over time, that characterizing how the human body adapts to spaceflight, in what direction do these systems go and why? And if we need a countermeasure, how do we develop them? And the other art of this is when you test a countermeasure, you definitely are looking for the outcome of interests, like you’ll have a hypothesis. Let’s just take something very tangible in terms of muscle loss. So we’re going to do resistive exercise, because we know that loading skeletal muscle will at least maintain skeletal muscle volume and strength. So our hypothesis is going to be if we can load somebody one hour a day, you know, with so many pounds or force, you know, we can achieve that. But what we also have to make sure is while we’re looking at that and testing that hypothesis that we look on the other side which is what risks could we be causing by doing the countermeasure. So your body does change in space, as I said. One of the things, and you hear about a lot, is people come back taller. You know, I think this gets tweeted about a bit.
Host: Yeah, like two inches or something.
Jennifer Fogarty: Yeah, it ends up being a couple centimeters, can be as much as, it can be as much as an inch or so. And what’s interesting is every day and night, our body goes through a lengthening and a shortening process. So at night, while you’re laying down, your spine kind of expands and it unloads, and you are a little taller in the morning when you stand up than you are when you go to bed at night. Because you compress yourself, because you’re vertical in gravity, and you got squishy stuff between each of your vertebrae and on the disks. And your body kind of settles down and you go through like this kind of cyclic nature. That’s a very normal process for your spine. But when crew members go into spaceflight, it’s not only laying down, but we said slightly head down would be kind of the feeling anyway. So your body gets unloaded for long periods of time. Well, your spine not only elongates, but it actually straightens. And there’s been a lot of reports of back pain over decades now of spaceflight. This really, we couldn’t understand why. Well, we think we finally figured it out and that as the spine straightens, all the muscles and ligaments that allow your spine to be, and your spine should be in an S-shape, well, when it’s straighter than the S-shape, those ligaments now are being stretched and muscles being stretched in a way that’s pretty uncomfortable while you’re adapting. Well, when you exercise, if we were to load somebody on their shoulders like in a squat, and now your spine is no longer that S-shape, it’s now more straight, we have a little potential for having, we think, a risk– an injury to your disks or your vertebra.
Host: Interesting.
Jennifer Fogarty: So we would carefully load somebody or change the way you would hold the bar. And we design exercise equipment, of course, so we could take into consideration that change. Because we want to get the benefit of the countermeasure and minimize or eliminate any risk. So we’re often, I think we talk about it a lot more on Earth when we talk about medications. You talk about the reason you’re taking the medication and the effective reason and then the side effects, you know, like how much side effects am I willing to tolerate to get the benefit? So each countermeasure has to be looked at in that way. So we have to make sure we pay attention to not only what we wanted it to do or what we thought it was going to do but the things we didn’t understand, like the unintended consequence. So that element is really designed to look across at all those things.
Host: Yeah, you need that deep focus because it’s not just OK, yeah, we’re going to do resistive exercise, because it goes a little bit deeper than that.
Jennifer Fogarty: Yeah, and if we’re going to do it, how do you do it safely to maximize benefit and minimize risk. So yeah, that’s really what they do. And it’s a very broad portfolio. Like I said, you’ll see gastrointestinal, immune, cardiovascular.
Host: Alright.
Jennifer Fogarty: Yeah, so they’re an exciting group, and they’ve got a lot of breadth and depth for sure.
Host: Yeah, I can’t wait to talk to them. We’ll take a deep dive with them too. Next one is research operations and integration.
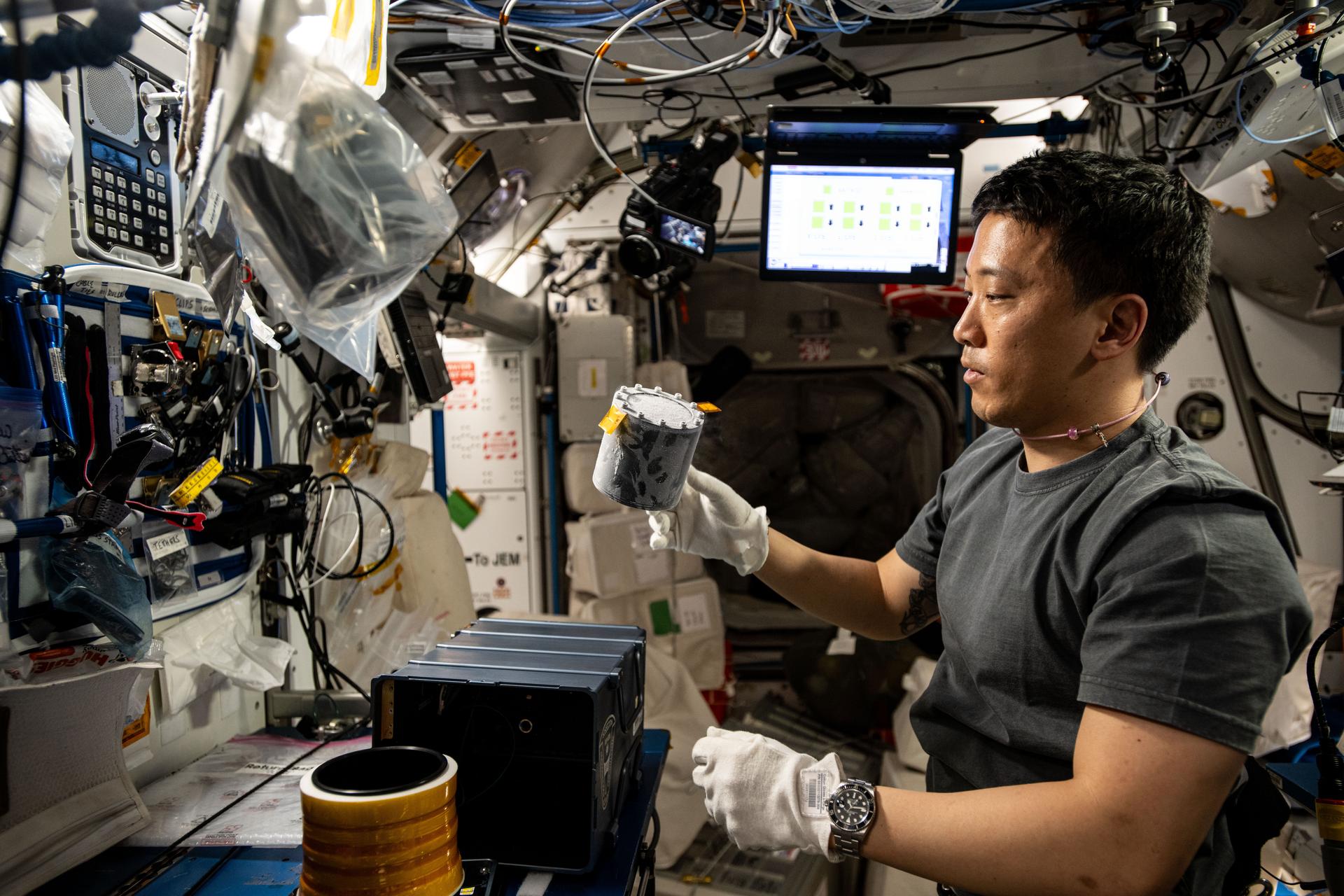
Jennifer Fogarty: Yeah, that is our implementing arms. So, one of the interesting parts of the work we do is doing science in space is incredibly challenging. You are probably not going to have most of the tools you’re traditionally used to having at your bedside if you’re a wet scientist. So this is the group of experts that really get us to the point where we can fly and experiment. And we have confidence that the experiment will produce results we can interpret. So we just talk about really like a type two error, which is, you know, getting a false negative. Those are things you really want to avoid. Like I just didn’t do my measurements correctly, and I missed the signal. False positives are another one, but those you can design to test for. So but this group is really a specialist in saying, how do we, if a development of hardware, how do we make it spaceflight worthy? How do we test it too into space? How do we launch it? How do we write procedure so that the crew can operate it and deploy it? Sometimes it’s medical testing. Like venipuncture, how do you take blood sample from yourself or each other? They do the crew training for that. They are also very helpful in managing blood volume. So lots of people right now I mentioned diving into the molecular world and omics. Omics relies on things like blood as a large staple of their resource to do their experiments. So, we have limits on how much blood we can take from each crew member per month. So they kind of, what we call it racking and sacking, we look across who’s in the flight queue for blood volume. What are the priorities? What are the objectives? And kind of have to decide how the blood volume is used. They also design the tubes or certify the tubes to fly. We can’t just fly any type of tube that you might get when you go get blood taken at your local phlebotomist. So they really do everything from the full life cycle of experimentation. They come in very early in our projects and do feasibility, so they tell us, you know, can this be flown this way or how much modification, how much hardware has to be built? They do the flight queue, and they also do what are called informed consent briefings of the crew, because they’re all test subjects so they volunteer for our science. So they pretty much coordinate all of that. They also coordinate the data streams back to the investigators so that they can receive their data. And they help us manage what are called data sharing. You know, before you mentioned data is good. Well, it’s even better when you don’t have to be the one who collects it. You just get to share it, you know, someone else is getting it. Plus it makes the data more valuable —
Host: Right.
Jennifer Fogarty: –and keeps the burden off of say the crew from collecting the same thing ten times. So, they work really hard at finding those types of efficiencies so that we are as, like as least invasive and as least obtrusive to the crew. So, because they have other science they have to do. They have other operations they have to do.
Host: And they don’t want their blood taken all the time.
Jennifer Fogarty: Not all the time. But they understand that bodily fluids are a precious resource, especially in astronauts. We make the best use out of them.
Host: That’s a great way to put it. Big job, definitely, on that end. That’s a big job. Let’s wrap it up with space radiation. This is another big one, right.
Jennifer Fogarty: Yeah, so space radiation is an interesting element. Not my background, so I’ve had to learn a lot about it in the past couple of years, more deeply than ever. So when I was on the operation side, it really was about safety in space. And we have a space radiation analysis group that monitors space weather that has a lot to do with the solar cycle. And there are different types of radiation in space, some that we don’t really have to deal with here on Earth because we’re protected by the magnetosphere. And the International Space Station has a pretty significant level of protection as well, not as good as we do, but it’s not like deep space will be. So that’s a whole different animal for sure from a radiation perspective. So the space radiation actually, before it became an element in HRP, was a program element. Actually, when I talked about like the bioastronautic roadmap, it actually was this other program element, wasn’t quite a big program P like ISS program, but it had its own life. And it was really dedicated using an Earth-based simulator at a Department of Energy facility that we use at Brookhaven National Laboratory. And a variety of experiments say what is the biological impact of these things that are called heavy ions, which again, are the particles that don’t make it through our atmosphere and kind of affect us. So we don’t really have any Earth-based data to tell us what is the biological relevance? But there are lots of unknowns about, we do understand humans and radiation from the gamma and x-ray perspective, you know. Those are a large resource of that data tells us epidemiologically what happens like after Hiroshima and Nagasaki has been a reference of populations as a, what happens to these humans, if they survive it, when do the different disease processes start to take place and how severe are those disease processes? So the big one that’s always discussed is cancer.
Host: Right.
Jennifer Fogarty: Right. And that’s a very common, and you can see the mental connection between something damaging your body in that way and turning a cell to a direction where it proliferates in an uncontrolled manner and becomes a cancerous source. So there’s a lot to be concerned about. But we are learning more and more about how we study it, to be honest. Recently, we just had advances made at the facility where they can do what’s called GCR, which is galactic cosmic rays, a simulation of it. And that means you can run a complex series of these heavy ion beams in your experiment, which is more similar– I guess that’s how –[Laughter]
Host: Yeah.
Jennifer Fogarty: more similar to deep space radiation than ever before. But we’re really excited about some opportunities with Gateway and the lunar opportunities to characterize and design experiments to study deep space radiation there that will give us the opportunity to validate all of the work we’ve done on the ground to be able to make I think stronger conclusions. The key thing there is understanding potential for countermeasures. So we work actually with a lot of folks who use radiation as a source of therapy for cancer treatments. So particularly proton therapy is of interest to us because the idea is they need and want to cure you of your cancer today, and they may use radiation to do that. But that may inadvertently give you a different cancer later in your life, because it’ll damage tissue in the surrounding area. So they want to prevent that in the future as well, the medical community does. So they are actually studying a lot of treatments that you would give at the time you receive that radiation therapy to protect the healthy tissue. So it’s one of those, again, just like we have that tension and have to struggle with choices of today about effects of tomorrow. So we are learning a lot from them that on a biological level, how can we protect people in general from radiation damage? So I think we’ve made some progress there, but we’re going to continue to invest in it. And that element will have definitely some interesting stuff to tell you.
Host: Yeah, I’m definitely seeing why there are these elements, why they’re organized the way they are and why you need such depth. You need those checks and balances, right, because you can come up with a solution, but you need to make sure that that’s a good solution. You mentioned the radiation example. You mentioned the countermeasure example when you’re in those workouts, you don’t want those negative effects. Moving to risks, you know, we’re talking about how, what happens to the human body. We want to understand that. We want to develop countermeasures for that to protect the humans and make them successful ultimately. But I know there are these risks that are identified. And there’s a number, there’s 33 risks that’s identified for human spaceflight. We don’t have to go through all 33, but in general, what do they tell us? What do they provide for the, you know, us understanding what questions to ask when doing human research?
Jennifer Fogarty: Yeah, so I think it is exactly that. It is a framework to help us get our arms around the human system within human spaceflight. So, there’s a lot of debate, and there has been for decades actually, more decades than you and I have been around for, about these risks. And even when I mention the bioastronautic roadmap, my very first meeting I went to, newly minted employee, was a bioastronautic roadmap meeting. And the whole thing was about what was called lumping and splitting. So when you have these risks, when you’re going to talk about the human, you can always group them in different ways, or you can split them out to be more and more sensitive or specific. And there’s always groups of thought that will pull you in one way or the other. But eventually, in order to get some work done, you kind of have to consent on a format that we’re just going to agree to, put our disagreements aside and say OK, given the lumping and the splitting that’s gone on, do these represent holistically a way that we can get at the totality of the human to know if we’re good to go to an exploration mission or not? So based on that evolution from bioastronautics roadmap to the Human Research Program was already that down select process. And I kind of mentioned a lot of vetting had gone on, a lot of external review had gone on that said that these really represented the biological systems in their totality. And that underneath each of those risks are many risk factors that if you really looked at you’re like OK, I can see how one, almost every risk is linked to one or more other risks, going back to even your countermeasure statement that there’s no one thing in your body when you think about the dials that if you turned it slightly that you wouldn’t be turning another dial that you’d better be keeping your eye on. So, it’s, again, there’s a lot of potential there for someone else to have a different perspective and articulate them differently. But I think the consensus is those represent the best holistic approach to covering the human system within spaceflight. We do structure them in a way that we use probabilistic risk assessment and another board process that gives us a likelihood and consequence. And that’s really where they get their priority ranking. And that says, there’s so much we either don’t know about this thing, and the consequences could be so severe that it’s going to get what’s called a red. And that really at this point from the Human Research Program and the agency perspectives, red is very typically communicated not unlike anyone else who uses red which is stop. It is a no go. Like this risk is not in a posture that’s acceptable, and we have a lot of work to do to get this into an acceptable risk posture so that we can fly. So you’ll see a group of red, like if you go to the HRP website, it’s a very transparent document that we use, and then there’s a group that are yellow, and those are caution. Those either say that we haven’t completely mitigated it or we don’t know enough about it to mitigate it completely. We’ve got open questions. But it’s not in the area of catastrophic outcomes that we’re saying that it’s a no go. It’s just there’s a lot of caution to be used there. And then we have risks that we think we’ve characterized enough, and we know good mitigation strategies that we call them green. And those are ones that we’ve kind of deprioritized, and I don’t want to kind of mischaracterize them. It’s not that we actually don’t do work on them, because they’re involved with the other risks. But they are not the primary target of reducing any further. A byproduct of a really good countermeasure for a red or a yellow could make a green even better. You’d want to make sure, going back to your earlier statement. You don’t want to inadvertently turn a green yellow or a green red by a countermeasure that you injected in another area. And so we’re constantly looking across the risks whenever we alter one. And remember, we’re doing this on paper right now. But there is usually data that tell you to crosstalk between risks, and you really have to pay attention to that. And there have been occasions where we would design or we would look for work that was designed to kind of pull out that kind of detail that helped us understand better the crosstalk between risk. Because sometimes it’s not so obvious, particularly in areas that are continually emerging like the immune system and the microbiome, of course, which doesn’t sit neatly in any one element, because it’s present throughout the body, can affect multiple systems, can be affected by multiple systems. So it doesn’t seem to have a start or a finish. It’s just always in the mix, so it has to be assessed even when you’re doing things you wouldn’t have anticipated. So if you’re doing understanding psychological stress, you would want to measure the immune system and the microbiome. If you think you’re going to give a nutritional supplement and improve the microbiome, you probably should measure output of behavior.
Host: They’re linked.
Jennifer Fogarty: Yeah, they’re linked. And there’s more and more data terrestrially to talk about behavioral disorders and the microbiome and treatments of the microbiome that have been very impactful to those behavioral disorders. And it’s very unexpected. They don’t, they can’t tell you how, but that’s one where a correlation is so strong it is verging on causality. They just can’t pinpoint the mechanism. And there is a thing called the gut brain axis to pay attention to. So how your mind works and how your GI tract works and vice versa. So that, again, probably hinges on the microbiome and a lot of messaging, whether it be chemical messages or hormonal messages. But they are definitely communicating with each other. And so any interventions that we do or test have to look at all of those systems simultaneously. And that’s the power of getting samples and sharing data that we don’t have to stand up a unique protocol for an experiment, but we can make sure that we have a standard protocol that’s used to give us a good reference point. And that’s something we instituted pretty recently which was called standard measures for that particular effort.
Host: Yeah.
Jennifer Fogarty: And is that we can gain a lot of efficiency this way, and we can also give a really good backstop of data of anyone doing anything experimental. So I think that’s how the risks have been approached. We review them annually, and we work with another board called the human system risk board that has a lot of what we call stakeholders here. A lot of people have a voice at the table to weigh in on the evidence base and how we’re calculating that likelihood by consequence and whether we’re doing more work or different work. So, it’s a very active part of our program, and it really determines kind of our priorities and how we go after the work that we do when we make our research announcements.
Host: There is so much to human research. I cannot wait to peel back the layers, but Jenn, what excites you about the future? Just everything we’ve talked about, you know, looking back, even looking back on all the human research since you came here in 2004 and what has progressed with human research just in that time. And then looking forward to, particularly Artemis, in the near future here and what we can look forward to for human research on the Moon.
Jennifer Fogarty: I think what’s so exciting is every time we discover anything about the human body, it points to the amazing resilience and robustness of the human condition. Given the right raw materials, the right support system, the right consideration, we’re a pretty amazing species. And I think we can rise to almost any challenge. I haven’t seen one yet. So, I just think that, to find the data and see the data really help us, you know, zero in on how to enable the crew of the future and the diversity of crew that can go. You know, the no limits. And some of the best outcomes have come from the most diverse participants. So I think it’s broken down all kinds of barriers and preconceived notions about who’s fit for spaceflight and who’s not. So Artemis, Artemis is opening up the window to deep space research for us that will give us a lot more confidence and ability to gain those insights about questions we’ve not been able to answer here on Earth because we just can’t simulate that environment. We’re trying to be really smart about it. I mean Artemis initially is going out as a very lean effort, landing people, and the first woman and the next man in 2024. I mean it’s a full court press to accomplish that, to get a lander on a sent module that we don’t have. So all resources are being put into accomplish that task. So we want to be on board. We want to be a great partner. We try to do things. So our key words are autonomous, light and lean. That’s what our requirements are, and that’s how we operate and kind of how MOD, which is our mission operations director that’s trained like to fly, so we do science like we want to fly, you know. You have to have a vision for how this thing will come together in the end. You know, what is that, how will it manifest, because that needs to be in your mind as you’re designing your way to get there. Because otherwise, you go a bit astray. You know, we have folks who want to do, you know, large devices, and everybody wants their own countermeasure. And you’re like this will not be an active operational solution. So it’s really integrating on all those complex challenges and results and going back to that picture where I don’t have the puzzle box in front of me. Each time you get a new piece, it’s really exciting to go back to the table and say where does this fit. What does it tell me about the other pieces I have here? Because it may cause a whole shift that I couldn’t have anticipated. We do a lot of work in the Antarctic. That’s been a real resource of some eye-opening isolation and confinement studies. So it’s been pretty exciting to see how that’s played a role. And that goes back again to like the immune system and things that look very much like station. We have human data from station, and we can find very similar human responses down the Antarctic, and people didn’t expect that. So, some of it’s not about being spaceflight per se, it’s about being that challenge, that stressful environment and the human condition. So it’s been an interesting equalizer along the way. But Artemis, yeah, definitely the challenge ahead of us, and it is definitely a Mars forward activity for us.
Host: Wonderful. Jenn Fogarty, this was a wonderful overview of all the human research and the history, current, future on everything human research. It was a pleasure talking to you today. Thanks for coming on.
Jennifer Fogarty: Yeah, it was my pleasure being here. Thank you very much.
[ Music ]
Host: Hey, thanks for sticking around. Really good conversation we had with Dr. Jenn Fogarty today about the overview of human research in space, the history, the future and everything in between. This is the first of a six-part series on the Human Research Program. There’s five more to go, and we’re going to dive deep into those elements. So I hope you stick around for those next five episodes. You can find us on NASA.gov/podcasts along with many other NASA podcasts that are out there. And if you really want to dive deep into human research right now, you just can’t wait for us, or you want to take part in some of the human research that’s being done all across NASA and across the world really, we’ll get into that over these next five episodes. Go to NASA.gov/hrp. Houston We Have a Podcast is on social media. We usually post on the Johnson Space Center pages of Facebook, Twitter and Instagram. Use the hashtag #askNASA on your favorite platform to submit an idea for the show if you’d like to have a topic come on. Just make sure to mention it’s for Houston We Have a Podcast. This episode was recorded on November 18th, 2019. Thanks to Alex Perryman, Pat Ryan, Norah Moran, Belinda Pulido, Brett Redden, Emmalee Mauldin and the Human Research Program team for helping to bring this all together. And thanks again to Dr. Jenn Fogarty for taking the time to come on the show. We’ll be back next week.