“Houston We Have a Podcast” is the official podcast of the NASA Johnson Space Center, the home of human spaceflight, stationed in Houston, Texas. We bring space right to you! On this podcast, you’ll learn from some of the brightest minds of America’s space agency as they discuss topics in engineering, science, technology and more. You’ll hear firsthand from astronauts what it’s like to launch atop a rocket, live in space and re-enter the Earth’s atmosphere. And you’ll listen in to the more human side of space as our guests tell stories of behind-the-scenes moments never heard before.
For episode 59, Dr. Erik Antonsen, element scientist and emergency physician, discusses the hazard of traveling farther away from Earth an ever before, especially how to provide appropriate medical care with limited resources and challenging communications. This is part three of a five-part series on the hazards of human spaceflight. This episode was recorded on June 28th, 2018.
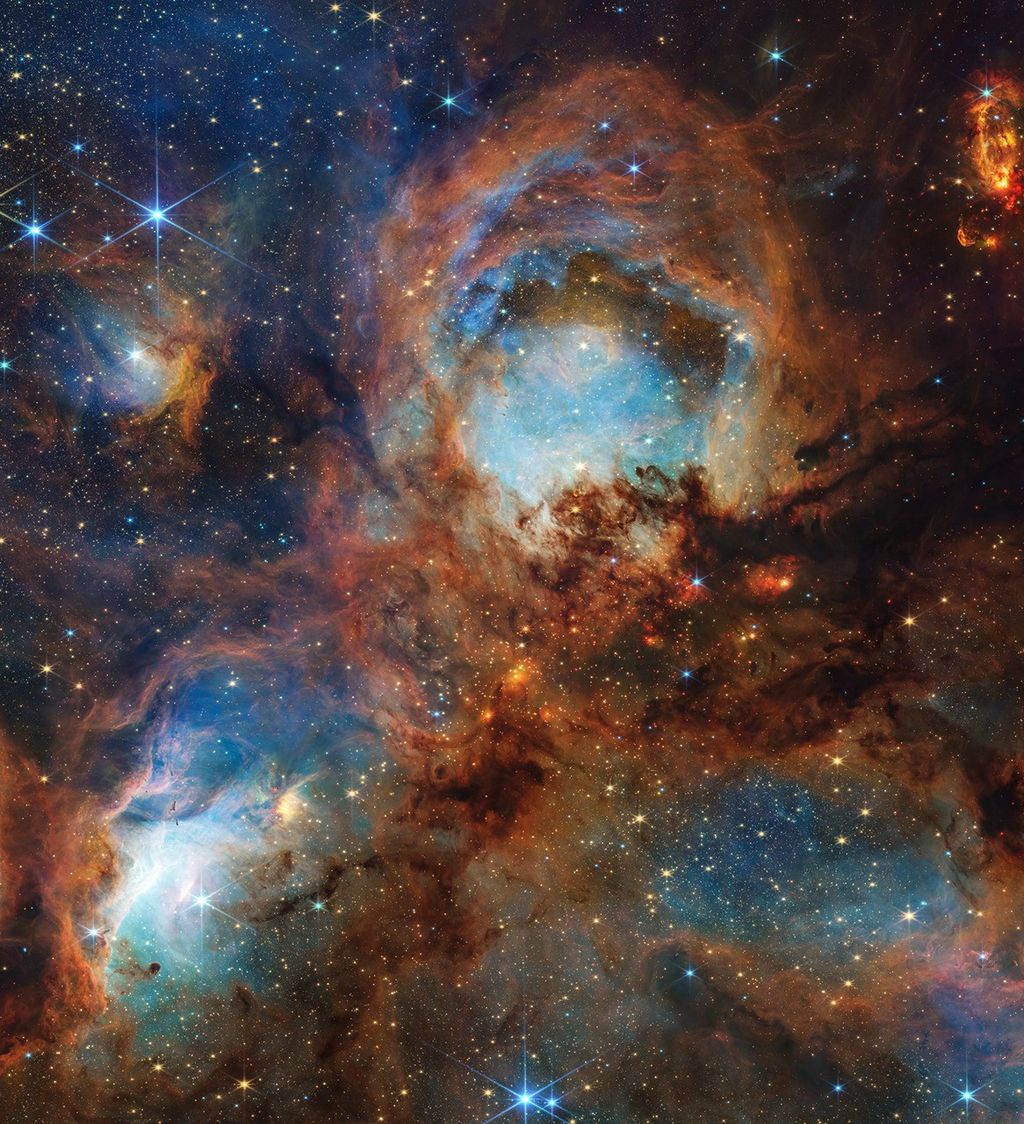
Exploration to the Moon and Mars will expose astronauts to five known hazards of spaceflight, including distance. To learn more, and find out what NASA’s Human Research Program is doing to protect humans in space, check out the “Hazards of Human Spaceflight” website.

Transcript
Gary Jordan (Host): Houston, We Have a Podcast. Welcome to the official podcast of the NASA Johnson Space Center, Episode 59: Distance. This is part three of our five-part series on the hazards of human spaceflight. I’m Gary Jordan, and I’ll be your host today. On this podcast we bring in the experts, NASA scientists, engineers, and astronauts all to let you know the coolest information about what’s going on right here at NASA. So today we consider another hazard of human spaceflight, the distance from Earth, with Dr. Erik Antonsen. Dr. Antonsen is currently the element scientist for exploration medical capabilities and the assistant director of human systems risk management at the NASA Johnson Space Center. He’s also an assistant professor of emergency medicine and space medicine at Baylor College of Medicine in Houston, Texas — a lot of medicines. And clinically he works as an attending emergency physician at Ben Taub General Hospital. His focus lies on the intersection between medicine and spaceflight. And he’s currently tasked with minimizing the risks associated with isolation during exploration-class missions and the inability to provide appropriate medical care.
But first I wanted to start off one last time with Dr. Mike Barratt, who as a NASA astronaut and former flight surgeon gave his own thoughts on the challenges that are presented when traveling far, far away.
Mike Barratt:Well, I think there’s many aspects to that. One, I have to kind of think about the medical issues that — we know our crews are going to be healthy when we launch them, and we’re going to do our best to keep them healthy during flight with countermeasures and diet and medical monitoring. But if an acute event happens, somebody, for instance, starts clutching their lower abdomen and peeing out blood, then we think there’s a kidney stone, you know, that could definitely happen.
Host:Oh.
Mike Barratt:So in this case, instead of getting a panic call to the ground, asking immediately to talk to the surgeon, what we may get is a report saying, “Crew member so and so was clutching their abdomen in very bad pain. We pulled out the ultrasound, we found a stone. We think it’s passing. We’ve given pain meds, and they’re resting comfortably.” That’s the kind of paradigm that we’re moving to so that the crew members, again, are able to respond to an event and handle it the best they can and give us reports and ask for advice, so to speak, consultation rather than real-time guidance. And that, again, is very exploration-oriented. And if we have a whatever settlement or colony or outpost on Mars, that’s the paradigm. So that begins with the exploration transit.
Host:Yeah, there’s a lot of factors that go into that. Now you’re not — you have to — you have another base of knowledge that you have to have as a baseline for wherever you go out. Because instead of calling immediately to the ground, like you said, and getting the aid, the knowledge of the experts on the ground instantly, now you have to know sort of what to deal with. And then that mentality of not working together, the mentality of doing it yourself and reporting the progress.
Mike Barratt:Which, truth be told, I think even crew members on station right now — we understand that we’re trying hard to produce science, and having more consultation with the ground is really important. But more crew autonomy is recommended by almost every crew who returns from station, partly to enhance the efficiency and partly for peace of mind. But it is something that crew members really, I think, naturally want and will move into quite nicely. I have to think I had a very small combustion event on the Space Station while I was up there, really almost non-consequential, but that piece of hardware on the Russian segment started billowing smoke and overheating. And, of course, we were able to immediately call to the ground. And they knew about it immediately because of smoke detectors and whatnot. And in this paradigm, it would have been a call back that maybe they would have found out between 8 and 22 minutes later that we had this little combustion event, we pulled circuit breakers, this is what we found. Everything is fine now. We replaced the part that was burning, and we are in normal ops recovery.
How was your day? So, again, that’s kind of the paradigm that we’ll get to with exploration.
Host:Thanks to Dr. Barratt for providing such great insight over these past few episodes. So with no further delay, let’s jump right ahead to our talk about the hazard of distance with Dr. Erik Antonsen. Enjoy.
[ Music ]
Host:Erik, thanks for joining me here today to talk about the distance from Earth.
Erik Antonsen:I appreciate you having me on.
Host:And this is — this is an interesting topic because it seems so obvious, right? Of course we’re going to be far away, but with that comes a series of very challenging things that we’re going to have to overcome to be successful. So from a broad perspective, if you were — if someone were to ask you, “Well, why is distance such a problem?” how would you start?
Erik Antonsen:It has to do with understanding the implications of what distance from Earth means. We have grown up in the space age sort of operating in a relatively close position to Earth for the entirety of our program. And the — we’ve had nine missions that have gone outside of low-earth orbit with humans on them. Those nine missions, the last time that happened was in 1972, right?
Host:Yeah.
Erik Antonsen:So there’s a question of sort of the corporate memory of how to do that. But there’s also a difference in scale and time for the missions that we’re talking about. Those missions were like camping trips.
[ Laughter ] We — we spent most of our time learning the skills that we needed to learn in low-earth orbit where we had some advantages, right? And those advantages from the Human Health and Performance side of the world really can be summed up as three things. One is if something really goes wrong with a crew member, you come back to Earth. You can evacuate them. And that’s a reasonably quick timeframe. Another one is that if you need to resupply something — consumables, medications, food, whatever it is — that you have a pretty reasonable chance at having a good supply chain for that. And then the last one is beyond evacuation and consumables, the ability to actually talk, right? Real-time communications is something that we rely on in the current operational paradigm, and most people don’t realize how much we rely on it. Everything that the crew does is scheduled down to the minute in many cases or at least the five-minute increment. And if they have a challenge with all the myriad of different things that they’re asked to be experts in and do on the Space Station right now, they get to reach back, right?
If there’s an anomaly, or something wrong, or they can’t quite figure out how to get this screw off, they get to reach back through the radio in real time and ask somebody, “Hey, why isn’t this working? Can you help me out?” Right? In the context of low-earth orbit, that means that a lot of their — the information that they have to rely on, the knowledge, the memory, and the ability to process that information is actually displaced from the crew members down to mission control where you have a bunch of people sitting in a room thinking about this, who all have a bunch of people behind them sitting in a room also thinking about this with immediate access to a lot of data that the crew members aren’t going to have. Now, take us out of that paradigm, right? Take us someplace far enough away from Earth where you have those three things challenged, you end up in a place where with Mars closest approach, you may have a one-minute — three minutes one-way delay in communication. And that’s just one way, right?
And at its farthest approach you’re talking about the speed of light taking 22 and a half minutes one way to get back to Earth. And so that ability, then, to reach back and talk to somebody and say, “Hey, what do I do about this thing that broke here?” You don’t have that real-time feedback anymore. Right? And it gets longer and longer and longer the further you go from Earth. When we’re around the moon, you still have reasonably close to real-time communications, and we can probably establish a logistics chain to get medicines, food, and other things that we need reasonably well, right? The thing that’s really impacted there is if somebody has a medical issue or a problem and they need to be evacuated, you’re no longer talking about, you know, a few hours to 36 hours down from low-earth orbit to definitive medical care. Now you’re talking about three days, maybe six days, maybe even longer depending on the orbit and the logistics of actually organizing these things.
So all of a sudden, instead of being able to rely on hey, if something bad happens, I can just take this crew member down to Earth and we can deal with it there, now you have to ask the question of how do I figure out in the really limited mass and volume that we have and potentially the limited data telemetry that we have going back and forth between Earth, how do we get enough information and support to our crews so they can make decisions and do just enough to keep somebody alive or stabilize them for that journey that’s going to take a much longer time than it did before?
Host:Yeah.
Erik Antonsen:And at Mars, if you don’t have that evacuation capability, you’re kind of in trouble, right? Because the size of the spacecraft and the amount of stuff that we can bring is only getting smaller.
Host:Right.
Erik Antonsen:Right? That’s one of the big challenges. We get less volume to put things in. We get less mass that we get to carry up there. For medical and human performance things, that can mean everything from the food nutrition that you eat to the medicines that you’d like to use, right? All of that sort of stuff, you have less room for it. But maybe even more importantly, the skillsets, right? How do you know when something’s a problem? And this is what terrestrial medicine struggles with, right? When you have somebody come to the emergency department, more often than what they’re really asking is, “Hey, I’ve got this thing,” either a rash on my skin or a pole sticking out of me or whatever it is, [Laughs] how big of a problem is this, and how dangerous is this, and how fast does it need to be addressed?
Host:The pole’s got to be a big one.
Erik Antonsen:I would think so. Some of these are intuitive, but some of them aren’t, right? I mean, think about when you go to the doctor, right? Something hurts in my belly, and I don’t know what to do about it, right? And it’s not going away.
Host:Right.
Erik Antonsen:And so that could be anything from I got some food poisoning from something I ate to my appendix is getting ready to burst, to my pancreas is inflamed, to my gallbladder is a problem, right? That’s a huge amount of knowledge that physicians and nurses and other healthcare professionals piece together to try to figure out, all right, am I worried about this or am I not?
Host:Yeah.
Erik Antonsen:And in a setting where you’re on the way to Mars, or even around the moon, you know, the decision to actually evacuate somebody or to try to have to intervene on something at the worst can mean loss of human life if we don’t plan correctly and at the best might mean screwing up a multibillion-dollar program that we spent a lot of money to put somebody there to do a mission that they no longer can do.
Host:Seems like — so you’re talking about these three things, right? We’re talking about these camping trips that — talking, resupplying. And these elements, it seems like I can just sum them up to autonomy is really what it comes down to, elements and — of autonomy in all of these procedures and the way that we do things. They’re not going to have the help that they have right now on the International Space Station as much.
Erik Antonsen:As much is the keyword there, right? Because it’s sort of figuring out what’s the appropriate degree of autonomy so that you’re not overdesigning a system, you’re not trying to do more than you have to do? But you do enough to make sure that the crew that you put in place has the knowledge, the skills, the abilities, all the things and the resources that they need to deal with the things that are most likely to happen or those things that are most likely to be preventable that, you know, we really should be able to deal with beforehand. That’s a huge amount of things, right? That’s a — that’s everything that could possibly go wrong in the human body is on the list. And how do you start — how do you start whittling that down? [Laughs] I mean, that’s a really big challenge.
Host:Yeah. So if you’re talking about a crew going to — let’s just say as part of the crew of a moon habitat — or let’s just say a Mars has been to the in this instance, I’m guessing you would probably want to vouch for a medical person, a medical expert as part of that crew.
Erik Antonsen:So right now in the standards that NASA has, for anything that’s considered a planetary mission, we have a requirement to have a physician-level crew member —
Host:There you go.
Erik Antonsen:— as part of that crew. But outside of planetary, if you’re talking about going to the moon, we don’t have that requirement, right? And — and that’s — it’s a judgment call, right? Where do you draw that line? It’s hard to say.
Host:Yeah.
Erik Antonsen:Right? We have been successfully flying people on the International Space Station for 18 years now, right? And there have been a lot of medical issues that you probably haven’t heard about. But there haven’t been, like, issues to the level of having to evacuate or having to, you know, consider surgery in-flight or things like that, right? But that’s also in a domain where we have things relatively controlled. So if you transpose that back to the Apollo missions, right, to the moon, we actually had a very well-known case with Fred Hayes on Apollo 13 —
Host:Yeah.
Erik Antonsen:— when he got sick, right? If you went to see the movie Apollo 13, you they that — that that character, that astronaut got very sick on the way back. And actually, getting a little bit of insight into the story around that is very instructive for how we would think about going back to the moon or how we would think about going further out. See, most people, when they think about the risks that humans face in spaceflight in long duration and outside the Earth’s magnetosphere, they focus on things like radiation. They focus on exercise, bone loss, all these sort of things. Sometimes isolation with the behavioral health issues. But it’s really hard to quantify what is likely to be the risk from the medical side of things? And so we do probabilistic risk analysis, and we look all the what has happened in spaceflight, we look at what has happened to the astronaut corps on the ground, and we build an evidence base that helps us to try to get our heads around what we think is likely to happen, right? And on Apollo 13, what we saw was a case that’s sort of a real-world check for how well we’re doing, right?
Host:Yeah.
Erik Antonsen:So interestingly, he had gotten a urinary tract infection, right? These are not very common for men on the ground. And there’s an anatomical reason why. They’re much more common in women than men because of the length of the urethra that women have, right? But in space, we actually find that that difference fall apart. It changes. We’ve have had urinary tract infections — actually a fair amount in men — up on the Space Station in the MIR program. And the reason why is because of what the spacecraft environment actually does to your body. When you go up in microgravity, all your fluids come up out of your legs, and it turns on your carotid baroreceptors, and it changes the way your kidneys work, and you start peeing out a lot of fluid. And so you get dehydrated, that’s one thing. And when they go up, they also end up having some neurovestibular challenges as the signals coming from their eyes get decoupled with the signals coming from their semicircular canals in their ears. So they get space motion sickness or nausea, right? And so they’ll take some medicines for that, which are — Phenergan is one example of them.
Those medicines can actually cause — one of the side effects that they cause is urinary retention, which can lead to urinary tract infections, right? And so there’s a few different factors that contribute to hey, why do these people get urinary tract infections in this domain? And the problem is once they get them, then you have to treat them, right? Crews, when they get retention, will go in and self-cath, which is not a comfortable things to think about. But this is actually part of the reality of being in a different environment like this.
Host:Oh.
Erik Antonsen:And guess what? That also potentially can introduce bacteria into the urinary tract, right?
Host:Huh.
Erik Antonsen:So when Fred Hayes had his problem, part of the reason why he had the problem was because he kept a condom catheter on too long that was supposed to collect urine.
Host:Oh.
Erik Antonsen:Right? A simple thing that could have been avoided. But then what happened is he got sicker. So as urinary tracts progress, most of the time we think of a UTI in terrestrial parlance as something you give a few pieces of antibiotics a couple of days and all of a sudden you’re better, right? But in men it’s not always that simple. So we try to figure out well, how bad is the infection, right? So for Fred, we had a heart rate monitor, and an increasing heart rate is one signal or one thing that we look at to say are they getting sicker or not getting sicker? And he was getting sicker. We had a thermometer, but it was broken. So we actually couldn’t tell if he had a fever or not. We had two different antibiotics that were on the spacecraft at the time, but when we cultured his urine when he got back, we actually found out that those antibiotics wouldn’t have worked, that the bug was resistant. It was a Pseudomonas aeruginosa strain that was resistant to the antibiotics. So if we would have tried to treat him with those antibiotics, they wouldn’t have helped, right? So what happens, then, is the urinary tract ascends and can get to the kidney and can cause sepsis.
And this is one of those things that is now you’ve got a very big problem that, if you were able to deal with it in the beginning when it was a small problem and keep it from becoming a big problem, you would have been much better off. So we were lucky with Fred in one sense, even though his spacecraft blew up and he, you know, nearly lost his life because of the problems with Apollo 13. He actually was lucky that he was already being evacuated back home. So once they got home, they were able to treat him with the full armamentarium of resources that they have at any hospital, right, and fix him. Transplant that to a crew that’s got three more months left to get to Mars, no ability to evacuate, you can’t actually put any new medicines on there if the ones that you have don’t work. If you had broken your thermometer, you wouldn’t even have insight into how bad he’s getting, right? So what we learned from that — and when we do our modeling sepsis and urinary sepsis is one of those conditions that we worry the most about — what we learn from that is we need to figure out how to plan medical and Human Health and Performance resources to try to deal with the things that are most likely to happen when they’re small problems, not when they’re big problems.
Host:So when this happened, you did the analysis and realized that the antibiotics that we had onboard wouldn’t have helped anyway. That begs the question well, which ones do you bring on board? How do you know what’s going to happen to a crew and what things you’re going to have to treat? And that’s got to be a huge challenge. Because finite resources is one thing. And like you said, if you want to go home, it’s going to be months until you actually can — if you don’t have the antibiotic at hand, it’s going to be months.
Erik Antonsen:Yeah, this is a big challenge. And one of the things that we do, it’s actually a very unique capability at NASA in the Human Health and Performance Directorate is we merged an engineering technique called probabilistic risk assessment with medical evidence-based medical needs. And so there’s a team called the integrated medical model that works on hey, let’s take all the instances and all the things that we know that have happened in human spacecraft as much as we can and we’ll put that into a database, right? And then we’re going to go and look at analog populations, like submariners and people who live in Antarctica, and see what happens with them. And maybe it’s not the same thing as spaceflight, but it’s a close approximation. Then we’re going to go look out at the terrestrial literature and see for the things that we know that have happened in spaceflight or things that have happened to our astronauts on the ground, let’s see how often those things happen, right? And you start building up an evidence base that allows you to get an incidence; how often do things occur? Right? And how often do they occur in our domain or in domains that are like that, right? And then you can start actually bring statistical tools to bear to start saying, all right, let’s look at what is most likely to happen, let’s start looking what the consequences of those things are, what capabilities we would need to deal with those things, what medications we would like to have.
And then you start building up massive databases of this information and process that — all that data. And you actually run Monte Carlo models to predict well, how many times is this likely to happen based on what we know from the past, right?
Host:Right.
Erik Antonsen:That gets you in the ballpark.
[ Laughter ]
Host:All that for a ballpark.
Erik Antonsen:It’s a huge amount of work just to get in a ballpark. But it’s an evidence-based ballpark.
Host:Yes.
Erik Antonsen:It’s not a single flight surgeon or somebody else sitting there saying, “Well, you know, I saw this one guy who had a urinary tract infection, so we should take this medicine instead of that one,” right? And this is the challenge of — of a growing and learning space program, right? Sixty years ago we were not even necessarily trying to collect a ton of data because we didn’t know what was going to be important, what wasn’t. It was just the challenge of getting there.
Host:Right, doing it and then figuring it out.
Erik Antonsen:Right? A huge the amount of risk really up in until today has been borne by the launch vehicle, the landing, right, Challenger, Columbia. And a huge amount of risk has not been the failure of the human system within those things, right? But as we go to this greater distance from Earth and longer missions because of that greater distance, that proportion of risk that we carry that is the human system likely to fail gets bigger and bigger and bigger. And the launch and the landing at the beginning and end of that mission makes up a smaller and smaller proportion of the total risk you carry. So part of what we’re doing with the ISS and other programs that we work on is to try to build up our understanding of how’s that human system likely to fail? What are the things that are most concerning that we need to deal with? And it’s not just medicine, right? This is behavioral health. When you put people into isolated chambers as a team for multiple years — if you remember the Biosphere II project, right, they had eight people for two years stuck in that container, and they ended up all hating each other [Laughs], which is not the team dynamics you really want to have when you’re trying to do one of the most challenging things that our species has ever done.
Host:Absolutely.
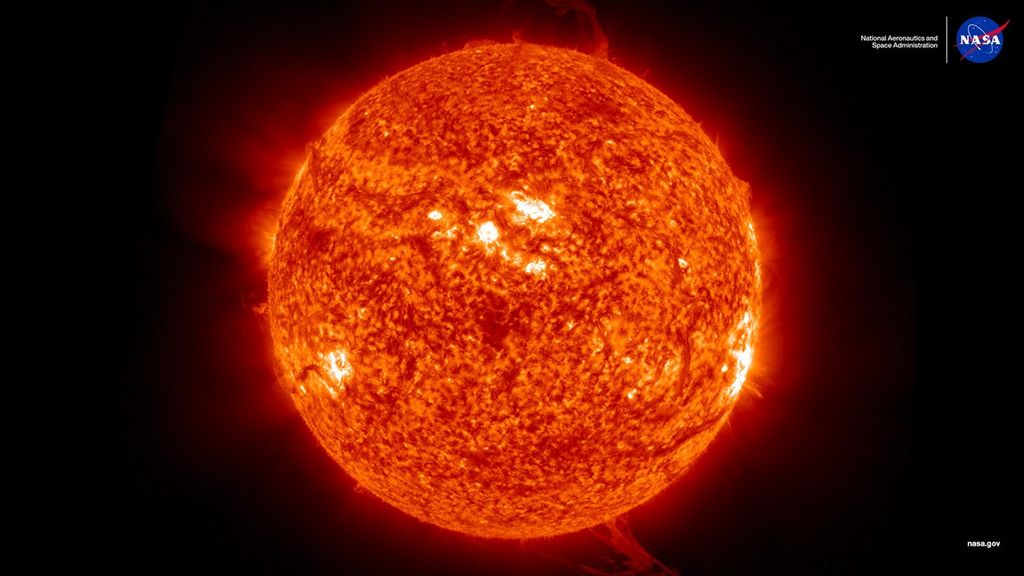
Erik Antonsen:So a lot of research that we do within this domain is to try to make sure that in the isolation and confinement that happens for this small tin can that we’re sending, you know, across the solar system, that we have an understanding of the ways in which people are going to suffer the stress, potential depression, challenges in social dynamics. And this is all behavioral health research that goes on at NASA, trying to inform those. In addition to that, that distance from Earth sort of hazard also crosses a line when we leave the magnetosphere and all of a sudden we have more and more radiation to worry about, right?
Host:Right.
Erik Antonsen:This is the one that everybody thinks of as a giant risk. And it’s a big risk, but it’s in addition to all these other things that we’re talking about. So all the different things that could go wrong start stacking up. And we spend a lot of time and effort trying to figure out, okay, how do we prioritize these things? How do we figure out what are the stuff that we really need to deal with? And how do we design systems so they are intuitive, so they help the crew with more autonomy, so they actually augment the crew? We’re not looking to replace the crew with an IBM Watson or something that’s like artificial intelligence.
Host:Sure.
Erik Antonsen:I think a lot of times people think that well, we could put Watson on this spacecraft and it might be able to replace the doctor. We don’t see that being something realistic anytime in the near future.
Host:Humans are too good?
Erik Antonsen:Humans are too good. And part of the purpose of human spaceflight is for us to explore and to — and to utilize those skills that humans have. We’ve already sent robots all over the space — all over the solar system, right?
Host:Yeah.
Erik Antonsen:This is the next wave. This is what happens when we try to go there and try to figure out how we do things, and how we function, and how we respond to this environment.
Host:That’s always the feedback I get. Because that’s a question that I love asking all my guests, really, is why do humans have to explore? And it’s that — I mean, you just can’t replace the perspective that you get from sending someone to another planet, or destination, or out in the universe in some thing.
Erik Antonsen:I think it’s actually more fundamental than that.
Host:Really?
Erik Antonsen:I don’t know that it’s you can’t replace it because you can’t right now — maybe someday in the future you could — bit it’s really that you wouldn’t want to.
[ Laughter ] It’s a prior assumption, right? We’re going there to learn not only about these places but also about ourselves, about our place in the universe, about how we respond and change. And we’re learning these things on the Space Station right now. When you talk about the things that happen in astronauts’ brains and their eyes and how they’re learning to accommodate to long-duration spaceflight what we’re really talking about is learning about us in a different environment and what happens, how do we do it? This — this group of astronauts that exists in this closed container, we’ve selected them to be really healthy people, right?
Host:Yeah.
Erik Antonsen:So if I’m thinking about clinical research and medicine and I want to ask a question about, you know, what happens if I have this one insult on a healthy person, right, these guys are a control group for an experiment that we as a species are doing, trying to understand how we learn about ourselves. So when we talk about loss of bone, loss of muscle, these are analogs for other diseases and things that can help us inform how we think about those diseases in terrestrial populations in ways that we’d never be able to do on the Earth.
Host:Now, this kind of leads nicely to — I’m going to kind of combine that with some of the previous statements you made about, you know, we’re talking about the supplies and your thoughts about what do we need to collect, what sort — you know, thinking antibiotics and medicines and supplies? But then also fitting that with a crew that’s going to work well together. If you’re thinking about going to a destination farther away, now you’re talking about, I guess, less and less space — livable space to do that. You know, we’ll have a transit vehicle that’s going to go out, and then we’re going to have a habitat, but those things — we’re really constrained by the mass that we can bring and the space that’s going to be available. And if you’re talking, you know, this group of eight people that hate each other after two years, you know, missions to Mars, they can be longer than that. So how do you know — how do you know what to bring and the masses that you — based on what you think, this is the medical supplies that we can bring that is going to sustain these people? But then also the people themselves, thinking about those things?
Erik Antonsen:You’re really talking about the merger of the science that we do, which is building up an evidence base and an understanding that we can draw from strong conclusions about what’s important and what’s not, what the size of effects are, and the relative proportion of things that are likely to happen, and the merger with engineering kind of in a systems engineering type of world, right? When you build a spacecraft, right, you have a whole bunch of different subsystems for that spacecraft that you got to accommodate. You have the structures to hold it all together; you have the propulsion system to push it all around; you have the power system to make sure that you can turn the lights on, turn the lights off, do whatever you need to do. Those are all sort of well understood piece parts of a vehicle. And then you also have this human system, right?
Host:Yeah.
Erik Antonsen:Which is the people, yes, but then all the things you need to keep the people alive, like the food, and the consumables, and the things that you’re talking about. And then also along with that, the monitoring and the tools that you need to understand the environment that they’re living in; is this staying within the parameters we like? The people themselves, are they staying within the parameters that we like? That’s where heart rate, and temperature, and some fundamental vital signs, and things like that are really important to know, right? And so it’s this gigantic smorgasbord of a lot of information that has to be put together in a systematic approach, right? And that’s why this is such a fascinating both scientific and engineering problem, right? We are trying to do something that’s never been done before in the history of our species. When I show slides that have, like, the solar system with the sun in the middle and the Earth and then Mars and their relative positions, and I talk about hey, the distance here, the distance that we’re going just to get to Mars, one of the things that I say is, “You see that little blue dot that is representing Earth?
At this scale on the solar system, our entire species, everything we’ve ever known is still within the size of that dot, even the visits to the moon are still within the size of that dot.” When I put it up with the Mars orbital distances, right?
Host:Right.
Erik Antonsen:Like, this has to have and has to involve the most rigorous, systematic, and disciplined approaches to both, you know, no kidding understanding what is happening to the human body in this domain and how it changes — the mind, the behavioral health issues, our response to the radiation environment, galactic cosmic rays, potential solar particle events, our likelihood of medical conditions occurring. You know, the risk that we buy down from selecting the healthiest people in the world has been great for low-earth orbit, but you get diminishing returns when you get out to three years. These people are not superhuman.
Host:Right.
Erik Antonsen:They’re still human, right? And so what you’re really talking about when you say, “How do we approach this problem?” well, some of that probabilistic risk analysis and modeling is part of it, but we’re still building the tools for a lot of these things. We’re still building models, we’re still building experiments. The Human Research Program is still trying to make sure that they make investments in places where they get results that inform positively do we care about this, is it really important, or should we move on to the next problem? Because we got a long line of problems that we have to challenge, right?
Host:Yeah. And you kind of alluded to this before — and this is — I’m going to bounce into a topic, you know, thinking about we have so many questions that we need to answer, but we are investigating things right now. So let’s go into that. You know, what do we know? What do we know right? And there’s been instances like you said before — you kind of hinted at this in beginning — there’s been, you know, medical things happening you said on MIR. What were some of the things that were happening? And then what did we do to resolve them real-time?
Erik Antonsen:Yeah. So there’s — there’s a variety of different things. And this actually feeds how well we validate some of the modeling that we do to try to predict the future. Right? You remember that there was one episode where there was a fire on MIR. And one of the medical issues that comes out of that is smoke inhalation. All of a sudden you got people inhaling smoke — maybe haven’t gotten to their mask in time or things like that. And now you have this exposure potentially toxic exposure that’s also causing them to cough and to, you know, not be able to function. And you have to make a decision about hey, do we actually, like, get out of here, right? Even if you contain the fire, if you’ve got a crew member who is incapacitated because of the results of that fire because of burns or because of smoke inhalation or something like that or, you know, maybe that fire damaged something like the ammonia lines and all of a sudden off toxic exposure, right, you have to try decide what do we do about that in real time? There were — there was at least one case of a cosmonaut who had a cardiac dysrhythmia who was disorbited from it. And — and we’ve seen changes in heart rhythm as we’ve gone through the space program.
There have been astronauts that had atrial fibrillation. The question mark is, like, is this something that, you know, we need to not have somebody fly for? Or all of a sudden, you know, they never had this problem, and you get into spaceflight and maybe they have it there. We actually haven’t seen any of that in the AmErikan cohort, but there was one Russian who was deorbited for it. And then there’s that question of, like, if you follow that to its logical conclusion, all right, that sort of explains why we do the biological monitoring that we do — heart rate, that sort of stuff. You see in Apollo 13 and other movies they have these pads on and you got a signal sending down to the ground. Sometimes your problem is you may actually have too much information and information that you don’t know what to do with. So a lot of what we continue to learn as we go forward is do we really want to know this? Right? And what I mean by that is something we find things in clinical medicine on the ground that we call incidentalomas, right? You go and you scan somebody’s head because they — you know, they got in a car accident and you’re worried about it. And you don’t find any evidence of trauma, but you find something there that you’re not sure what to do with that wasn’t bothering them before.
Now that can set off a chain of events. Do we have to go look at that further? Do we have more specialists involved? Does somebody get poked and prodded? Do we start causing more problems than we solve because we saw this thing that we don’t know what the significance is? And that happens in terrestrial medicine all the time.
Host:Right.
Erik Antonsen:Now transplant that to the spaceflight environment where something happened. We measured something, we don’t know if this is a big problem or not. Are we going to do more harm than good to a crew member or to a team by chasing after it, or should we wait and see? Right? That’s a challenge. This is in the clinical world. In my job in emergency medicine I run into this a lot, right?
Host:Yeah.
Erik Antonsen:What’s the appropriate amount of concern that I should have for somebody who’s really healthy, highly functioning, not having any problems? And then there’s this thing, a CT scan or an ultrasound that was found, right?
Host:Yeah. And it sound like a judgment call based on the physician on the ground. But the problem is now you’re not getting as much data as we go further away, correct?
Erik Antonsen:And so you now find that line, which is where the science and the art of doing these things meets, right? I mean, in clinical medicine today, right, we don’t know everything. There’s still lots — huge — amounts of clinical trials going on that inform us and update us on what the best things to do are for our patients. It’s no different in spaceflight. As we go longer and learn more, we incorporate the corporate memory that we’ve had from the past and the things that we’re learning there to update what we’re doing. But at some point you’re operating in a domain where you don’t have a huge amount of evidence to influence what you do. And this is where flight surgeons and operational support have to make judgment calls. And that is that line between science and art of how you actually do these things. And that’s the beautiful thing about this job is that you live in that domain where we’re constantly pushing the boundaries of what we know and how we understand it in the larger system of what we’re doing. And you get to build the science to help inform the art.
Host:So I’m guess we have a lot of — a lot of practice with the International Space Station now?
Erik Antonsen:So you’ve got 18 years of people being up there.
Host:Right.
Erik Antonsen:That — it’s interesting. When people bring up, “Hey I have this concern,” right? Radiation is going to turn bacteria into these horrible, mutant, virulent beasts, and people are going to get sicker than they’ve ever gotten before. And then you look at the Space Station, and yeah, we swab the surfaces and we measure this stuff. And we have scientists here look at samples and all that sort of stuff. And yeah, there’s some stuff growing up there that, you know, you don’t want to hear about. But at the same time in 18 years, you’ve never really had somebody get sick from those particular bacteria or those things growing. You’re not having this epidemic of astronauts, you know, all of a sudden, you know, ending up incapacitated because there’s some fungus or some mold growing in the corner, right? And so it’s that — that’s part of what informs the judgment, right, is hey, how do square the science and the things that we’re learning about the way genetics, and bacteria, and viruses get modified in this new environment, and our own body’s immune systems changes, and our T-cells drop over time when we’re in microgravity and low-earth orbit?
And what are the consequences of that? And then you look up at the clinical level and you say, “Well, nobody’s really getting that sick, so how much do I have to care?” That’s great, six months. We’ve got a pretty good establishment of that.
Host:Yeah.
Erik Antonsen:I’m not too worried about it. Three years with all three of those things that we were talking about earlier no longer being available. How comfortable do we feel extending that sort of experience-based judgment calls and the art side of this out into that domain? And that’s what helps us guide where we put our research investments in the science is to help inform that for these longer, and longer, and longer duration things that we’re looking to do.
Host:Which is a lot of what we’re doing on the Space Station is learning what we learn here, we get to kind of package and then take out. Obviously there’s going to be things we’re going to have to learn along the way. But it’s a pretty good model, especially operationally whenever we’re doing things day-to-day. I did want to circle back, though, to you said there’s stuff growing on the Space Station, you know, all the time. But 18 years, not really a concern. What’s growing, and how come medically we’re okay?
Erik Antonsen:Well, this is, like, if you think about your house on Earth, right?
Host:Yeah.
Erik Antonsen:And you can certainly find websites and companies that want to go clean up all the fungus and the mold in your house. And maybe at some point you get to a point where that stuff actually starts to bother the people in your house or you have people who start having allergic reactions, but, you know, it’s really not a different thing than there. There’s fungus, there’s bacteria. There’s a variety of bacteria that we bring on our skin everywhere we go. Right? And some of these are the most common bacterias that we worry about in terms of infections, right? Staphylococcus aureus is a naturally occurring colonizing species on your skin — we all have it.
Host:Eww.
Erik Antonsen:I know, I’m sorry. Staphylococcus, right, when you think about strep throat, these things live on our skin, right? They don’t really actually cause problems for us until they get into someplace where they’re not supposed to be, like, for example, if somebody gets a cut and all of a sudden, like, bacteria from the skin is now down in the bloodstream or in the subcutaneous tissue and all of a sudden, you know, maybe you get an infection there. If you’re really healthy, you probably don’t. In terrestrial medicine the places where we see this is people with diabetes and with suppressed immune systems and stuff like that, right? That’s where we really worry about it in terrestrial medicine. But hey, when we’ve measured the T-cells in our own immune system in flight, we’ve seen some changes there. We see the T-cells decreasing over time in the microgravity environment. So where is that point at which hey, we’re kind of approaching an immune suppressed status and we might need to worry about this more? In the case of these six-month missions, we haven’t reached that point, which makes us feel good, right? That’s — that’s helpful. But at a year or two years as we stretch that out, do the T-cells keep dropping or do they threshold and plateau someplace?
If think threshold and plateau someplace, maybe it won’t be a problem with all the bacteria we brought up. Maybe our body can handle it because it normally can. But I don’t know if they plateau or if it keeps going down and then you’re going to have a problem in two and a half years right at that point you’re on your way back from Mars but you still have long enough to go that you could get really sick and not be able to do much about it. And by the way, all those medicines you brought with you? If we look at the formulary on the International Space Station right now, about 16% of those medications that are on the International Space Station could within the labeled expiration dates actually make a trip out to Mars and back.
Host:That’s good to know.
Erik Antonsen:So on the way back, if you still have three months to go, most of your medicines, they may not work if we were just using what we had on the Space Station today.
Host:So what do we do to extend the life?
Erik Antonsen:That’s a good question [Laughs]. That’s one of the areas that when I was working for exploration medical capabilities, we laid out a pharmacy research plan to try to address just that stuff, right?
Host:Right.
Erik Antonsen:Some medications seem to be affected by the spaceflight environment. We’ve left stuff up there for about 880 days and we’ve seen increased degradation rates in what we call the API’s — the active pharmaceutical ingredients — compared to stuff that’s on the ground, right, controls that we look at. And it’s hard to suss out why. Maybe some of it’s radiation, maybe some of it’s the environment, some other things. But what we’re trying to get heads around is are there biochemical categories of medications that make more sense to rely on because other ones break down faster in that environment? Some things that are happening in the pharmaceutical industry in terms of, you know, adding additives to pharmaceutical makeups can actually extend those expiration dates; can we take advantage of those sort of things? Do we try to make medicines that instead of having to take twice or three times a day for ten days for your antibiotic course, you take once, right? NASA doesn’t do that stuff, but we look to the pharmaceutical industries and the advances that they take to try and pull intelligently the things that are going to extend our pharmacy and make it more functional over the timeframes we’re talking about.
Host:Yeah. Now, this — this kind of goes back to you talking about, you know, what happens after six months? Does it plateau or does the immune functionality continue to decrease? What knows? But my assumption would be if it does, if we do have to worry about possibly go — decreasing — now maybe you’re taking more medication, now maybe you’re being extra careful where if you do get a cut, oh, you want to patch that up immediately because you don’t want anything getting in. Now you’re talking about using more resources.
Erik Antonsen:And having to bring more to be able to enable that.
Host:Right.
Erik Antonsen:Which we don’t have a lot of volume for.
Host:Right.
Erik Antonsen:It’s this — this ultimate backpack game, right?
Host:Yeah.
Erik Antonsen:How do you build up the best understanding of what changes are going to happen and being impactful? So you only bring the things that really matter. Like, right now we have a defibrillator up on the Space Station, and it’s an ongoing source of discussion, right? You’re familiar with the defibrillator like in the airport? You put it on, you shock somebody’s heart if their heart were to stop.
Host:Clear, yeah.
Erik Antonsen:Clear, bzzt [Laughs].
Host:Right.
Erik Antonsen:The whole — the whole point of that sort of thing is that when the heart enters certain electrical rhythms that don’t pump blood, you stun it and reset it, right? But what you’re really talking about, the underlying problem before that and after that is what’s wrong with this person that their heart actually entered that? And most of the things that would lead to that are stuff we screen for and get out of the way in the astronaut corps, right? So we don’t really expect them to be in a position where they’re probably going to need that. The likelihood of it happening is extremely low. And so if you’re really up against the wall in terms of the volume, does it make sense to bring that, right?
Host:Right.
Erik Antonsen:I don’t know because it’s a really, really, really low likelihood event, but it’s really high consequences if it happens. But part of the way we answer that is by looking at all right, what else comes with that? If you actually shock somebody, it doesn’t mean they’re automatically okay, right? This is not TV. [Laughs] It means that you’ve got a whole bunch of other work to do and a whole bunch of other resources to bring to bear to do resuscitation on somebody who’s really sick. And the odds of us being able to supply those sort of things in this small volume and space is really, really small, right? So now you start asking the question, “Is that a risk we’re willing to take?” And it’s a challenge.
Host:Yeah. Because now you think about oh man, but what if we do need it, right? But you’re saying — you’re pretty confident based on we’ve flown so many times and we’ve gotten, you know — if you’re thinking back to Fred Hayes, back to that time, we were kind of figuring out spaceflight. That was the whole point of Mercury, and Gemini, and Apollo is to keep going further and kind of figure it out along the way. Now we’ve done it a lot. We kind of know what we need to do before a spaceflight to make that spaceflight successful medically too. So yeah, maybe you can kind of take it away and feel confident learning from these operations.
Erik Antonsen:To paraphrase Frank Borman when he was sitting in front of Congress, right, the places that we’re going to fail after this much time are the places where we have a failure of imagination, right? It’s the things that we didn’t know about that are going to come and bite us. And there’s going to be enough of those. So we have to intelligently plan for the things that we do know about. If something is really, really low likelihood, we probably need to be making room for things that are much more high likelihood that will help to us make sure that we don’t let those small problems, the little cuts to the skin, the infection in the urine, the other things like that grow into the big problems that all of a sudden we’re never going to be able to provide the resources to handle if it reaches something like a sepsis level.
Host:Do you find that, you know, meeting with other doctors and other people in your field, getting together, you’re still coming up with more questions that needs to be answered?
Erik Antonsen:I would say that all good science lead to more questions.
[ Laughter ] That’s just the reality of the world in which we live, right? As soon as you start nailing down something in the evidence base, you immediately have the question of wait, but what if this happens or what if our assumptions about this weren’t correct? How does that change what we would do? And that’s an ongoing conversation and question that we have with the flight surgeons, and the research doctors, and the research scientists, and the immunologists, and the toxicologists, and the systems engineers? Like, this is what the ongoing conversation is that occurs between the people doing a lot of the research in these areas and the people who are doing operations right now for the programs that we have set up. I mean, SS is the most big and visible of them.
Host:Sure.
Erik Antonsen:But there’s other things that are happening — the commercial crew programs and how we interface with those guys, Orion’s coming up, and then soon to be Gateway. Like, these are all going to have unique challenges. And everybody that’s got experience to bring to bear, they have a piece of the puzzle for figuring out how to do it safely and how to do it right. Right? And then there’s also people who are working in field that we haven’t had to pull on yet that are going to have other pieces of the puzzle. So how to do it safely and how to do it right?
Host:Now I know, I mean, just personally working with large groups, you get a lot of different input and diversity of thought, which is good. But then you have everyone providing so much input that you can’t agree on anything.
Erik Antonsen:At some point you got to make a decision [Laughs]. How does that happen?
Host:That was going to be my question. How do you — I mean, you do want as much information as possible. Because that’s how you’re going to be successful. But then how do you — how do you know which things to sacrifice? You know, you’re already talking about a defibrillator. How do you know which things to sacrifice to come to an agreement on this is the most important elements of what’s going to make a mission successful?
Erik Antonsen:Yeah, so part of this question is really wrapped in what at NASA or who at NASA makes decisions, right, after they have looked across all this stuff? So there’s a couple of different places. I work with the Human Health and Performance directorate. My job right now is assistant director for humans systems risk management. And one of those parts of that job is to chair the human systems risk board. I started that a couple months ago, it’s actually a new job for me.
Host:Oh, cool.
Erik Antonsen:But the purpose of the board is to look across all the risks that we have to try to assess the evidence base to understand, hey, how big of a problem is this, how well do we understand what as going on, how well do we expect to know what’s going on in a few years, you know, and how do we prioritize where we should put our investments? And that board is a wide group of people who look at these problems from a bunch of different angles. And they come together and no kidding, no everybody goes away happy all the time. But it’s one of those hey, we got to have a transparent and open discussion about what the puts and the takes are when we’re looking at these programs and how we’re funding our research going to the future. And so that board actually flows out of the Health and Medical Technical Authority. There’s three technical authorities at NASA that were founded after the Columbia accident. When they were looking at what were the pressures that teams that were looking at the risks and the challenges and the science of what they were doing — what pressures were they facing just because the agency had goals and they were sometimes pushing on people to meet them, right?
Host:Sure.
Erik Antonsen:So what they did was they established three independent reporting lines. People who had no dog in the fight for actually getting and meeting program schedules. One of those is an engineering technical authority. One of them is a safety and mission assurance one. And the third one is a Health and Medical Technical Authority. And it derives its power from the chief medical officer and headquarters at NASA. But the responsibility of that group is look at the risks, look at the evidence base, look across all of these problems and start prioritizing. Right? And start making some of those hard decisions about if we’re going to make standards that we hold future programs to and requirements about whether or not you’re going to have a defibrillator or something else, right, that those — those things have an open and vigorous debate about the benefits and the costs potentially, the risks of including this and not including that.
Host:Yeah.
Erik Antonsen:And so we’re always working to try to improve how much information we bring to bear, how we actually communicate, right? It’s very easy for technical people in these fields to speak with jargon and to potentially leave other experts who are, you know, as accomplished in completely different fields sitting there, thinking, like, they’re idiots because I don’t understand what this person is saying.
Host:Right.
Erik Antonsen:So you’re talking when we come to these boards, what we’re talking about is bringing expertise, and engineering, and spacecraft, and systems engineering together with medical doctors, together with life scientists. And all of them are speaking their own languages, all right? It’s a big challenge. So this past year, the former chief medical officer — guy named Rich Williams from NASA — actually commissioned a book called the Rosetta Stone. It’s a handbook for trying to get life scientists, fit medical doctors, and engineers to understand each other’s perspective and the language they speak in. Because we’re always trying to figure out how do you take people who have a huge amount of insight and understanding in this field over here and get them to understand what the problems are in a different field? That communication is a massive challenge.
Host:Absolutely. Oh, I want to check that out, too. Because that would be probably good across the board just communicating with folks that maybe speak a different language than you.
Erik Antonsen:Yeah, we just published that one a couple months ago.
Host:Nice. Well, focusing on that, now you said you’re focusing on human systems risk management, but you also are actively practicing emergency medicine. So with that comes a certain perspective when it comes to what you bring to the table. So what are some of the things that you’ve been bringing to the table recently?
Erik Antonsen:So I maintain practice in emergency medicine up at Ben Taub. I’m professor at Baylor. And NASA actually buys my services from Baylor as a professor. The — my perspective is informed by what do I do in emergency medicine in my practice today? And maybe even more so, what would I rather have been done so that somebody didn’t have to show up in the emergency room, right, the preventative aspect of care?
Host:Captain Hindsight.
Erik Antonsen:I get a lot of opportunities to say, “Man, it would have been great if you would have just done this or known that or, you know, and the system had this sort of thing plugged in.”
Host:Right.
Erik Antonsen:And that’s part of it. The other half of my background is I was a PhD engineer, aerospace engineer in propulsion. I used to do that for the Air Force Research Laboratory. So I spent a lot of time both as a medical doctor kind of dealing with the realities of the sickest people that we see in Houston — Ben Taub is a level one trauma center. It’s a lot of indigenous, immigrant, uninsured population that we deal with there. So people who have not had the primary and preventive care we would like to see, and therefore they end up in emergency rooms more often than not. And then I also have spent time as an engineer for spaceflight, looking at how propulsion systems mesh with the larger vehicle systems. And so when I look at the problem of human system risk, I’m looking at it from the what’s the right answer on the medical side hopefully to prevent the problems that I see and deal with in my practice? But how do you make that jive with the realities of the engineering life cycle of designing a vehicle? Right? One of the biggest oversights that the physicians have in the flight surgeon cadre who have never been exposed to an engineering design life cycle is they don’t even know what the words mean, right?
Host:[Laughs] Goes over my head.
Erik Antonsen:These spacecraft, when you’re starting to build a spacecraft, right, you have different phases that engineers all understand — prephase A, phase A, phase B. You don’t actually fly one until you get to phase E. And prephase A can start a decade before you actually build this thing. Right?
Host:Wow.
Erik Antonsen:So when you’re actually designing and creating the requirements that a Boeing, or the NASA engineers, or SpaceX, or somebody’s going to go build this spaceflight do, you kind of need to know what you need to get it into the mix at least five years and sometimes longer ahead of time.
Host:Wow.
Erik Antonsen:Now, contrast that with what happens in the medical world in technology development, right? All of a sudden we have this explosion of innovation in the medical world. What we’re learning and how we use things like iPhones, which didn’t exist when I was in grad school, right, or even in medical school, like, the technology that we are able to bring to bear on understanding the human system just for terrestrial medicine right now is changing so rapidly that if I said, “I want to use this thing in five years for my medical practice,” I would be doing my patients in five years a severe disservice.
Host:Right [Laughs].
Erik Antonsen:Right?
Host:You can’t do it.
Erik Antonsen:So now think about the Space Station, right? It’s 2018, we’ve been having people up there since 2000. The first module went up in 1998. The design freezes that occurred for what was going to be included on this vehicle in the year 2018 happened probably three to five years before 1998, right? I got my first cell phone of any kind in 1998 [Laughs], right? The ways in which we handle data and expect things from our technology are completely different today than they were then, right? We don’t have automatic means of capturing a lot of information up on the Space Station and the things that we do have are fixes we’ve made after the fact. So when we talk about designing something like the Gateway vehicle or, like, what’s going to take us to Mars and you’re trying to figure out what the right things to include are today, knowing that that mission may not happen for five to ten years, but if you don’t actually put placeholders and things in there, then the engineers aren’t going to actually keep volume and mass for your stuff, right?
And this is the problem. What we have on the Space Station today in terms of a medical system is good. We have an environmental health monitoring system. We have a health maintenance system, which is some medical kits with equipment and supplies and medicines. And we have a countermeasure system, which involves exercise equipment that we’ve changed over time, right? None of the data from any of those things is connected. Right now if you wanted to know for your, like, fitness how well you’re doing on keeping up with your stuff, you’d use your Apple Watch, or your MyFitnessPal on your phone, or something to track your job in the park. And you could, like, see how you’re doing over time, right?
Host:Yeah.
Erik Antonsen:None of that stuff was designed into the Space Station. But it’s an expectation on the data that we have for today in the world that we operate with that we’re at least going to have that sort of interoperability with the things that we send on a crew to Mars. But remember, NASA’s been operating and optimizing a system for the last 18 years that hasn’t needed that. So it’s actually a shift, a big shift in the way we think about the way we do business in low-earth orbit. We have put up some things like apps with iPhones and iPads — not iPhones but iPads. And sometimes we’ve learned things that were surprising. Like, the certificates for the Apple iPad and the apps that they have, they don’t — since they don’t have a direct connection to the Cloud, all of a sudden your iPad’s going to stop working after a certain amount of time.
Host:Oh.
Erik Antonsen:Yeah. So now you got to accommodate in the networking that you do for the vehicle. And we still have problems with it. We’ve ran into it for the last several years. It’s those type of small problems that we learn in a systems engineering sense and in a data management sense in the Space Station today that we need to make sure don’t happen on the way to Mars. Right? So we’re learning in every aspect. It’s not just how the human body changes but even how we do data, how we set up our networks, how all this stuff talks to each other. And when we get into that place where we all of a sudden no longer have any real-time communications and you need to put that ultrasound on somebody and go look at their appendix or their kidney or something, and you don’t have somebody to guide you and tell you which way to point the probe, you better have included a learning module that shows them how and where to look and how to interpret the images.
Host:Yeah. So being conscious of your time, I’m just going to ask you one more thing: If you had to take something — just based on what we’ve discussed today — and let’s say we have a long-term presence on the moon, some folks that are practicing some of these things that we need to explore further out into the solar system, Mars being one of the destinations, what are some of the things that you are looking forward to trying on the moon?
Erik Antonsen:So there’s a giant list.
[ Laughter ] Part of it is actually managing the data that we have and learning how to do that with a different ground support model than we currently have today. Because those are the first steps of what’s going to enable us to change from the ISS paradigm and the everything readily available paradigm over to something that’s going to be appropriate to going to Mars. That’s one way that we learn to do the mix of monitoring the human system that we worry about, along with making sure that we can be supportive in whatever ways we can be. Another thing is we don’t have a dose response curve for gravity and what happens with the human body. Right? Those T-cells that I told you about declining?
Host:Yeah.
Erik Antonsen:I don’t know if that’s isolation, stress, radiation, microgravity, right? You put somebody on the moon, all of a sudden you have a data point at one-sixth gravity, right? We don’t know the neurovestibular changes that happen. We don’t know how long they’re going to last when you go into one-sixth gravity. We don’t know how well the body’s going to accommodate in one-sixth gravity compared to microgravity, right? Or three-eighths at Mars, right? So part of spending time on the surface of the moon from the perspective of the human and how we change is starting to get another data point somewhere between no gravity and the three-eighths gravity that we expect on Mars. And right now all we’ve got is 1G and zero, right? So that’s a really amazing opportunity to start collecting data in a partial gravity environment and start building that dose response curve to what happens to the whole accommodation, right? You’ve heard of the sands problem, sometimes called VIP, where they have the eyeball changes, and some astronauts have had changes in their vision and need to wear glasses and that sort of thing?
How’s that going to change when you put partial loading back on the body? When you actually have the fluids in the body pulled back down again. But maybe not that much, right? It’s a whole new set point for adaptation that we’re not going to understand that until we spend some time there doing it, right? We didn’t have enough chance in the ’70s when we were at the moon to really start kind of gauging those questions.
Host:Right, they were camping trips.
Erik Antonsen:We’ve got basic functionality, right? Can we do this? Can you walk around? What happens if you fall over, right? And also we learned that astronauts would hurt themselves in creative ways [Laughs]. You know, when we do our modeling for the loads that people experience and we’re worried about hey, are these guys to break their bones because of the changes in their bone density and stuff like that? Most of the modeling of loads that we would expect to be applied says no, it’s too low of a load in these gravitational fields. And yet one of the astronauts, you know, managed to go out there, get a piece of equipment stuck in the ground, and then trying to get it out, stuck his shoulder up underneath it and really hurt himself pushing up against it, right? It’s those sort of things that oh, I didn’t know that person was going to do that. I probably should be aware of that and take that into concern or into my calculations for what I provide, right? [Laughs] It could be anything from, like, potentially fracturing a bone to pulling a muscle, to just having a bruise. We don’t know, but it sort of reminds us that when we think we have solutions and we think we have answers, humans have a wonderful way of surprise us.
Host:Yeah. It’s those extra data points that are really going to be — really going to help us out. But then just learning along the way, what questions do we still need to ask?
Erik Antonsen:Yeah. Right now we’re comfortable with the evacuation times we have from the Space Station. What happens when we’re living in that domain where it takes three days? How do we change the way we view medicine? How do we change the way we view prevention? How do we change the way that we support our crews as we get farther and farther away from Earth? As that distance increases, the question marks just multiple. So that’s one more set of data points and ways in which we can start to understand the real impact of that hazard, which is distance from Earth.
Host:I can’t wait to find out.
Erik Antonsen:Me, too.
Host:Erik, thanks for coming on the podcast today and sharing your perspective on what it takes to go far, far away.
Erik Antonsen:I appreciate you having me. Thank you.
[ Music ]
Host:Hey, thanks for sticking around. So today we talked with Dr. Erik Antonsen. We talked about being far from Earth, the distance from Earth, and all the challenges that come with it. This is part of our series of the five hazards of human space flight. We’ve had several podcast episodes so far — two down, I guess this is our third, and two more to go. We are actually partnering with the Human Research Program to do this series. So they have a video series and animations that are paired with each of these episodes. You can go to NASA.gov/hrp to see those videos and the content that’s supplemented with these five hazards and the three that we’ve done so far. For the International Space Station, you can go to NASA.gov/iss. A lot of the research we talked about today is on board the International Space Station. So you can go to that website to find out some of the research going on there. Otherwise you can follow us on social media. It’s Facebook, Twitter, and Instagram for the International Space Station or the NASA Johnson Space Center accounts. Go to those, whatever platform is your favorite, and use the hashtag #AskNASA to submit an idea for the show.
Just make sure to mention it’s for Houston, We Have a Podcast and we might make a whole episode out of it. So this podcast was recorded on June 28th, 2018. Thanks to Alex Perryman, Pat Ryan, Bill Stafford, Nell Whiting, Bill Polaski, Judy Hayes, Isidro Reyna, Mel Whiting, and Thalia Patrinos. Thanks again to Erik Antonsen for coming on the show. We’ll be back next week with the fourth of the five hazards of human space flight, discussing altered gravity fields. See you then.
Gary Jordan (Host): Houston, We Have a Podcast. Welcome to the official podcast of the NASA Johnson Space Center, Episode 59: Distance. This is part three of our five-part series on the hazards of human spaceflight. I’m Gary Jordan, and I’ll be your host today. On this podcast we bring in the experts, NASA scientists, engineers, and astronauts all to let you know the coolest information about what’s going on right here at NASA. So today we consider another hazard of human spaceflight, the distance from Earth, with Dr. Erik Antonsen. Dr. Antonsen is currently the element scientist for exploration medical capabilities and the assistant director of human systems risk management at the NASA Johnson Space Center. He’s also an assistant professor of emergency medicine and space medicine at Baylor College of Medicine in Houston, Texas — a lot of medicines. And clinically he works as an attending emergency physician at Ben Taub General Hospital. His focus lies on the intersection between medicine and spaceflight. And he’s currently tasked with minimizing the risks associated with isolation during exploration-class missions and the inability to provide appropriate medical care.
But first I wanted to start off one last time with Dr. Mike Barratt, who as a NASA astronaut and former flight surgeon gave his own thoughts on the challenges that are presented when traveling far, far away.
Mike Barratt:Well, I think there’s many aspects to that. One, I have to kind of think about the medical issues that — we know our crews are going to be healthy when we launch them, and we’re going to do our best to keep them healthy during flight with countermeasures and diet and medical monitoring. But if an acute event happens, somebody, for instance, starts clutching their lower abdomen and peeing out blood, then we think there’s a kidney stone, you know, that could definitely happen.
Host:Oh.
Mike Barratt:So in this case, instead of getting a panic call to the ground, asking immediately to talk to the surgeon, what we may get is a report saying, “Crew member so and so was clutching their abdomen in very bad pain. We pulled out the ultrasound, we found a stone. We think it’s passing. We’ve given pain meds, and they’re resting comfortably.” That’s the kind of paradigm that we’re moving to so that the crew members, again, are able to respond to an event and handle it the best they can and give us reports and ask for advice, so to speak, consultation rather than real-time guidance. And that, again, is very exploration-oriented. And if we have a whatever settlement or colony or outpost on Mars, that’s the paradigm. So that begins with the exploration transit.
Host:Yeah, there’s a lot of factors that go into that. Now you’re not — you have to — you have another base of knowledge that you have to have as a baseline for wherever you go out. Because instead of calling immediately to the ground, like you said, and getting the aid, the knowledge of the experts on the ground instantly, now you have to know sort of what to deal with. And then that mentality of not working together, the mentality of doing it yourself and reporting the progress.
Mike Barratt:Which, truth be told, I think even crew members on station right now — we understand that we’re trying hard to produce science, and having more consultation with the ground is really important. But more crew autonomy is recommended by almost every crew who returns from station, partly to enhance the efficiency and partly for peace of mind. But it is something that crew members really, I think, naturally want and will move into quite nicely. I have to think I had a very small combustion event on the Space Station while I was up there, really almost non-consequential, but that piece of hardware on the Russian segment started billowing smoke and overheating. And, of course, we were able to immediately call to the ground. And they knew about it immediately because of smoke detectors and whatnot. And in this paradigm, it would have been a call back that maybe they would have found out between 8 and 22 minutes later that we had this little combustion event, we pulled circuit breakers, this is what we found. Everything is fine now. We replaced the part that was burning, and we are in normal ops recovery.
How was your day? So, again, that’s kind of the paradigm that we’ll get to with exploration.
Host:Thanks to Dr. Barratt for providing such great insight over these past few episodes. So with no further delay, let’s jump right ahead to our talk about the hazard of distance with Dr. Erik Antonsen. Enjoy.
[ Music ]
Host:Erik, thanks for joining me here today to talk about the distance from Earth.
Erik Antonsen:I appreciate you having me on.
Host:And this is — this is an interesting topic because it seems so obvious, right? Of course we’re going to be far away, but with that comes a series of very challenging things that we’re going to have to overcome to be successful. So from a broad perspective, if you were — if someone were to ask you, “Well, why is distance such a problem?” how would you start?
Erik Antonsen:It has to do with understanding the implications of what distance from Earth means. We have grown up in the space age sort of operating in a relatively close position to Earth for the entirety of our program. And the — we’ve had nine missions that have gone outside of low-earth orbit with humans on them. Those nine missions, the last time that happened was in 1972, right?
Host:Yeah.
Erik Antonsen:So there’s a question of sort of the corporate memory of how to do that. But there’s also a difference in scale and time for the missions that we’re talking about. Those missions were like camping trips.
[ Laughter ] We — we spent most of our time learning the skills that we needed to learn in low-earth orbit where we had some advantages, right? And those advantages from the Human Health and Performance side of the world really can be summed up as three things. One is if something really goes wrong with a crew member, you come back to Earth. You can evacuate them. And that’s a reasonably quick timeframe. Another one is that if you need to resupply something — consumables, medications, food, whatever it is — that you have a pretty reasonable chance at having a good supply chain for that. And then the last one is beyond evacuation and consumables, the ability to actually talk, right? Real-time communications is something that we rely on in the current operational paradigm, and most people don’t realize how much we rely on it. Everything that the crew does is scheduled down to the minute in many cases or at least the five-minute increment. And if they have a challenge with all the myriad of different things that they’re asked to be experts in and do on the Space Station right now, they get to reach back, right?
If there’s an anomaly, or something wrong, or they can’t quite figure out how to get this screw off, they get to reach back through the radio in real time and ask somebody, “Hey, why isn’t this working? Can you help me out?” Right? In the context of low-earth orbit, that means that a lot of their — the information that they have to rely on, the knowledge, the memory, and the ability to process that information is actually displaced from the crew members down to mission control where you have a bunch of people sitting in a room thinking about this, who all have a bunch of people behind them sitting in a room also thinking about this with immediate access to a lot of data that the crew members aren’t going to have. Now, take us out of that paradigm, right? Take us someplace far enough away from Earth where you have those three things challenged, you end up in a place where with Mars closest approach, you may have a one-minute — three minutes one-way delay in communication. And that’s just one way, right?
And at its farthest approach you’re talking about the speed of light taking 22 and a half minutes one way to get back to Earth. And so that ability, then, to reach back and talk to somebody and say, “Hey, what do I do about this thing that broke here?” You don’t have that real-time feedback anymore. Right? And it gets longer and longer and longer the further you go from Earth. When we’re around the moon, you still have reasonably close to real-time communications, and we can probably establish a logistics chain to get medicines, food, and other things that we need reasonably well, right? The thing that’s really impacted there is if somebody has a medical issue or a problem and they need to be evacuated, you’re no longer talking about, you know, a few hours to 36 hours down from low-earth orbit to definitive medical care. Now you’re talking about three days, maybe six days, maybe even longer depending on the orbit and the logistics of actually organizing these things.
So all of a sudden, instead of being able to rely on hey, if something bad happens, I can just take this crew member down to Earth and we can deal with it there, now you have to ask the question of how do I figure out in the really limited mass and volume that we have and potentially the limited data telemetry that we have going back and forth between Earth, how do we get enough information and support to our crews so they can make decisions and do just enough to keep somebody alive or stabilize them for that journey that’s going to take a much longer time than it did before?
Host:Yeah.
Erik Antonsen:And at Mars, if you don’t have that evacuation capability, you’re kind of in trouble, right? Because the size of the spacecraft and the amount of stuff that we can bring is only getting smaller.
Host:Right.
Erik Antonsen:Right? That’s one of the big challenges. We get less volume to put things in. We get less mass that we get to carry up there. For medical and human performance things, that can mean everything from the food nutrition that you eat to the medicines that you’d like to use, right? All of that sort of stuff, you have less room for it. But maybe even more importantly, the skillsets, right? How do you know when something’s a problem? And this is what terrestrial medicine struggles with, right? When you have somebody come to the emergency department, more often than what they’re really asking is, “Hey, I’ve got this thing,” either a rash on my skin or a pole sticking out of me or whatever it is, [Laughs] how big of a problem is this, and how dangerous is this, and how fast does it need to be addressed?
Host:The pole’s got to be a big one.
Erik Antonsen:I would think so. Some of these are intuitive, but some of them aren’t, right? I mean, think about when you go to the doctor, right? Something hurts in my belly, and I don’t know what to do about it, right? And it’s not going away.
Host:Right.
Erik Antonsen:And so that could be anything from I got some food poisoning from something I ate to my appendix is getting ready to burst, to my pancreas is inflamed, to my gallbladder is a problem, right? That’s a huge amount of knowledge that physicians and nurses and other healthcare professionals piece together to try to figure out, all right, am I worried about this or am I not?
Host:Yeah.
Erik Antonsen:And in a setting where you’re on the way to Mars, or even around the moon, you know, the decision to actually evacuate somebody or to try to have to intervene on something at the worst can mean loss of human life if we don’t plan correctly and at the best might mean screwing up a multibillion-dollar program that we spent a lot of money to put somebody there to do a mission that they no longer can do.
Host:Seems like — so you’re talking about these three things, right? We’re talking about these camping trips that — talking, resupplying. And these elements, it seems like I can just sum them up to autonomy is really what it comes down to, elements and — of autonomy in all of these procedures and the way that we do things. They’re not going to have the help that they have right now on the International Space Station as much.
Erik Antonsen:As much is the keyword there, right? Because it’s sort of figuring out what’s the appropriate degree of autonomy so that you’re not overdesigning a system, you’re not trying to do more than you have to do? But you do enough to make sure that the crew that you put in place has the knowledge, the skills, the abilities, all the things and the resources that they need to deal with the things that are most likely to happen or those things that are most likely to be preventable that, you know, we really should be able to deal with beforehand. That’s a huge amount of things, right? That’s a — that’s everything that could possibly go wrong in the human body is on the list. And how do you start — how do you start whittling that down? [Laughs] I mean, that’s a really big challenge.
Host:Yeah. So if you’re talking about a crew going to — let’s just say as part of the crew of a moon habitat — or let’s just say a Mars has been to the in this instance, I’m guessing you would probably want to vouch for a medical person, a medical expert as part of that crew.
Erik Antonsen:So right now in the standards that NASA has, for anything that’s considered a planetary mission, we have a requirement to have a physician-level crew member —
Host:There you go.
Erik Antonsen:— as part of that crew. But outside of planetary, if you’re talking about going to the moon, we don’t have that requirement, right? And — and that’s — it’s a judgment call, right? Where do you draw that line? It’s hard to say.
Host:Yeah.
Erik Antonsen:Right? We have been successfully flying people on the International Space Station for 18 years now, right? And there have been a lot of medical issues that you probably haven’t heard about. But there haven’t been, like, issues to the level of having to evacuate or having to, you know, consider surgery in-flight or things like that, right? But that’s also in a domain where we have things relatively controlled. So if you transpose that back to the Apollo missions, right, to the moon, we actually had a very well-known case with Fred Hayes on Apollo 13 —
Host:Yeah.
Erik Antonsen:— when he got sick, right? If you went to see the movie Apollo 13, you they that — that that character, that astronaut got very sick on the way back. And actually, getting a little bit of insight into the story around that is very instructive for how we would think about going back to the moon or how we would think about going further out. See, most people, when they think about the risks that humans face in spaceflight in long duration and outside the Earth’s magnetosphere, they focus on things like radiation. They focus on exercise, bone loss, all these sort of things. Sometimes isolation with the behavioral health issues. But it’s really hard to quantify what is likely to be the risk from the medical side of things? And so we do probabilistic risk analysis, and we look all the what has happened in spaceflight, we look at what has happened to the astronaut corps on the ground, and we build an evidence base that helps us to try to get our heads around what we think is likely to happen, right? And on Apollo 13, what we saw was a case that’s sort of a real-world check for how well we’re doing, right?
Host:Yeah.
Erik Antonsen:So interestingly, he had gotten a urinary tract infection, right? These are not very common for men on the ground. And there’s an anatomical reason why. They’re much more common in women than men because of the length of the urethra that women have, right? But in space, we actually find that that difference fall apart. It changes. We’ve have had urinary tract infections — actually a fair amount in men — up on the Space Station in the MIR program. And the reason why is because of what the spacecraft environment actually does to your body. When you go up in microgravity, all your fluids come up out of your legs, and it turns on your carotid baroreceptors, and it changes the way your kidneys work, and you start peeing out a lot of fluid. And so you get dehydrated, that’s one thing. And when they go up, they also end up having some neurovestibular challenges as the signals coming from their eyes get decoupled with the signals coming from their semicircular canals in their ears. So they get space motion sickness or nausea, right? And so they’ll take some medicines for that, which are — Phenergan is one example of them.
Those medicines can actually cause — one of the side effects that they cause is urinary retention, which can lead to urinary tract infections, right? And so there’s a few different factors that contribute to hey, why do these people get urinary tract infections in this domain? And the problem is once they get them, then you have to treat them, right? Crews, when they get retention, will go in and self-cath, which is not a comfortable things to think about. But this is actually part of the reality of being in a different environment like this.
Host:Oh.
Erik Antonsen:And guess what? That also potentially can introduce bacteria into the urinary tract, right?
Host:Huh.
Erik Antonsen:So when Fred Hayes had his problem, part of the reason why he had the problem was because he kept a condom catheter on too long that was supposed to collect urine.
Host:Oh.
Erik Antonsen:Right? A simple thing that could have been avoided. But then what happened is he got sicker. So as urinary tracts progress, most of the time we think of a UTI in terrestrial parlance as something you give a few pieces of antibiotics a couple of days and all of a sudden you’re better, right? But in men it’s not always that simple. So we try to figure out well, how bad is the infection, right? So for Fred, we had a heart rate monitor, and an increasing heart rate is one signal or one thing that we look at to say are they getting sicker or not getting sicker? And he was getting sicker. We had a thermometer, but it was broken. So we actually couldn’t tell if he had a fever or not. We had two different antibiotics that were on the spacecraft at the time, but when we cultured his urine when he got back, we actually found out that those antibiotics wouldn’t have worked, that the bug was resistant. It was a Pseudomonas aeruginosa strain that was resistant to the antibiotics. So if we would have tried to treat him with those antibiotics, they wouldn’t have helped, right? So what happens, then, is the urinary tract ascends and can get to the kidney and can cause sepsis.
And this is one of those things that is now you’ve got a very big problem that, if you were able to deal with it in the beginning when it was a small problem and keep it from becoming a big problem, you would have been much better off. So we were lucky with Fred in one sense, even though his spacecraft blew up and he, you know, nearly lost his life because of the problems with Apollo 13. He actually was lucky that he was already being evacuated back home. So once they got home, they were able to treat him with the full armamentarium of resources that they have at any hospital, right, and fix him. Transplant that to a crew that’s got three more months left to get to Mars, no ability to evacuate, you can’t actually put any new medicines on there if the ones that you have don’t work. If you had broken your thermometer, you wouldn’t even have insight into how bad he’s getting, right? So what we learned from that — and when we do our modeling sepsis and urinary sepsis is one of those conditions that we worry the most about — what we learn from that is we need to figure out how to plan medical and Human Health and Performance resources to try to deal with the things that are most likely to happen when they’re small problems, not when they’re big problems.
Host:So when this happened, you did the analysis and realized that the antibiotics that we had onboard wouldn’t have helped anyway. That begs the question well, which ones do you bring on board? How do you know what’s going to happen to a crew and what things you’re going to have to treat? And that’s got to be a huge challenge. Because finite resources is one thing. And like you said, if you want to go home, it’s going to be months until you actually can — if you don’t have the antibiotic at hand, it’s going to be months.
Erik Antonsen:Yeah, this is a big challenge. And one of the things that we do, it’s actually a very unique capability at NASA in the Human Health and Performance Directorate is we merged an engineering technique called probabilistic risk assessment with medical evidence-based medical needs. And so there’s a team called the integrated medical model that works on hey, let’s take all the instances and all the things that we know that have happened in human spacecraft as much as we can and we’ll put that into a database, right? And then we’re going to go and look at analog populations, like submariners and people who live in Antarctica, and see what happens with them. And maybe it’s not the same thing as spaceflight, but it’s a close approximation. Then we’re going to go look out at the terrestrial literature and see for the things that we know that have happened in spaceflight or things that have happened to our astronauts on the ground, let’s see how often those things happen, right? And you start building up an evidence base that allows you to get an incidence; how often do things occur? Right? And how often do they occur in our domain or in domains that are like that, right? And then you can start actually bring statistical tools to bear to start saying, all right, let’s look at what is most likely to happen, let’s start looking what the consequences of those things are, what capabilities we would need to deal with those things, what medications we would like to have.
And then you start building up massive databases of this information and process that — all that data. And you actually run Monte Carlo models to predict well, how many times is this likely to happen based on what we know from the past, right?
Host:Right.
Erik Antonsen:That gets you in the ballpark.
[ Laughter ]
Host:All that for a ballpark.
Erik Antonsen:It’s a huge amount of work just to get in a ballpark. But it’s an evidence-based ballpark.
Host:Yes.
Erik Antonsen:It’s not a single flight surgeon or somebody else sitting there saying, “Well, you know, I saw this one guy who had a urinary tract infection, so we should take this medicine instead of that one,” right? And this is the challenge of — of a growing and learning space program, right? Sixty years ago we were not even necessarily trying to collect a ton of data because we didn’t know what was going to be important, what wasn’t. It was just the challenge of getting there.
Host:Right, doing it and then figuring it out.
Erik Antonsen:Right? A huge the amount of risk really up in until today has been borne by the launch vehicle, the landing, right, Challenger, Columbia. And a huge amount of risk has not been the failure of the human system within those things, right? But as we go to this greater distance from Earth and longer missions because of that greater distance, that proportion of risk that we carry that is the human system likely to fail gets bigger and bigger and bigger. And the launch and the landing at the beginning and end of that mission makes up a smaller and smaller proportion of the total risk you carry. So part of what we’re doing with the ISS and other programs that we work on is to try to build up our understanding of how’s that human system likely to fail? What are the things that are most concerning that we need to deal with? And it’s not just medicine, right? This is behavioral health. When you put people into isolated chambers as a team for multiple years — if you remember the Biosphere II project, right, they had eight people for two years stuck in that container, and they ended up all hating each other [Laughs], which is not the team dynamics you really want to have when you’re trying to do one of the most challenging things that our species has ever done.
Host:Absolutely.
Erik Antonsen:So a lot of research that we do within this domain is to try to make sure that in the isolation and confinement that happens for this small tin can that we’re sending, you know, across the solar system, that we have an understanding of the ways in which people are going to suffer the stress, potential depression, challenges in social dynamics. And this is all behavioral health research that goes on at NASA, trying to inform those. In addition to that, that distance from Earth sort of hazard also crosses a line when we leave the magnetosphere and all of a sudden we have more and more radiation to worry about, right?
Host:Right.
Erik Antonsen:This is the one that everybody thinks of as a giant risk. And it’s a big risk, but it’s in addition to all these other things that we’re talking about. So all the different things that could go wrong start stacking up. And we spend a lot of time and effort trying to figure out, okay, how do we prioritize these things? How do we figure out what are the stuff that we really need to deal with? And how do we design systems so they are intuitive, so they help the crew with more autonomy, so they actually augment the crew? We’re not looking to replace the crew with an IBM Watson or something that’s like artificial intelligence.
Host:Sure.
Erik Antonsen:I think a lot of times people think that well, we could put Watson on this spacecraft and it might be able to replace the doctor. We don’t see that being something realistic anytime in the near future.
Host:Humans are too good?
Erik Antonsen:Humans are too good. And part of the purpose of human spaceflight is for us to explore and to — and to utilize those skills that humans have. We’ve already sent robots all over the space — all over the solar system, right?
Host:Yeah.
Erik Antonsen:This is the next wave. This is what happens when we try to go there and try to figure out how we do things, and how we function, and how we respond to this environment.
Host:That’s always the feedback I get. Because that’s a question that I love asking all my guests, really, is why do humans have to explore? And it’s that — I mean, you just can’t replace the perspective that you get from sending someone to another planet, or destination, or out in the universe in some thing.
Erik Antonsen:I think it’s actually more fundamental than that.
Host:Really?
Erik Antonsen:I don’t know that it’s you can’t replace it because you can’t right now — maybe someday in the future you could — bit it’s really that you wouldn’t want to.
[ Laughter ] It’s a prior assumption, right? We’re going there to learn not only about these places but also about ourselves, about our place in the universe, about how we respond and change. And we’re learning these things on the Space Station right now. When you talk about the things that happen in astronauts’ brains and their eyes and how they’re learning to accommodate to long-duration spaceflight what we’re really talking about is learning about us in a different environment and what happens, how do we do it? This — this group of astronauts that exists in this closed container, we’ve selected them to be really healthy people, right?
Host:Yeah.
Erik Antonsen:So if I’m thinking about clinical research and medicine and I want to ask a question about, you know, what happens if I have this one insult on a healthy person, right, these guys are a control group for an experiment that we as a species are doing, trying to understand how we learn about ourselves. So when we talk about loss of bone, loss of muscle, these are analogs for other diseases and things that can help us inform how we think about those diseases in terrestrial populations in ways that we’d never be able to do on the Earth.
Host:Now, this kind of leads nicely to — I’m going to kind of combine that with some of the previous statements you made about, you know, we’re talking about the supplies and your thoughts about what do we need to collect, what sort — you know, thinking antibiotics and medicines and supplies? But then also fitting that with a crew that’s going to work well together. If you’re thinking about going to a destination farther away, now you’re talking about, I guess, less and less space — livable space to do that. You know, we’ll have a transit vehicle that’s going to go out, and then we’re going to have a habitat, but those things — we’re really constrained by the mass that we can bring and the space that’s going to be available. And if you’re talking, you know, this group of eight people that hate each other after two years, you know, missions to Mars, they can be longer than that. So how do you know — how do you know what to bring and the masses that you — based on what you think, this is the medical supplies that we can bring that is going to sustain these people? But then also the people themselves, thinking about those things?
Erik Antonsen:You’re really talking about the merger of the science that we do, which is building up an evidence base and an understanding that we can draw from strong conclusions about what’s important and what’s not, what the size of effects are, and the relative proportion of things that are likely to happen, and the merger with engineering kind of in a systems engineering type of world, right? When you build a spacecraft, right, you have a whole bunch of different subsystems for that spacecraft that you got to accommodate. You have the structures to hold it all together; you have the propulsion system to push it all around; you have the power system to make sure that you can turn the lights on, turn the lights off, do whatever you need to do. Those are all sort of well understood piece parts of a vehicle. And then you also have this human system, right?
Host:Yeah.
Erik Antonsen:Which is the people, yes, but then all the things you need to keep the people alive, like the food, and the consumables, and the things that you’re talking about. And then also along with that, the monitoring and the tools that you need to understand the environment that they’re living in; is this staying within the parameters we like? The people themselves, are they staying within the parameters that we like? That’s where heart rate, and temperature, and some fundamental vital signs, and things like that are really important to know, right? And so it’s this gigantic smorgasbord of a lot of information that has to be put together in a systematic approach, right? And that’s why this is such a fascinating both scientific and engineering problem, right? We are trying to do something that’s never been done before in the history of our species. When I show slides that have, like, the solar system with the sun in the middle and the Earth and then Mars and their relative positions, and I talk about hey, the distance here, the distance that we’re going just to get to Mars, one of the things that I say is, “You see that little blue dot that is representing Earth?
At this scale on the solar system, our entire species, everything we’ve ever known is still within the size of that dot, even the visits to the moon are still within the size of that dot.” When I put it up with the Mars orbital distances, right?
Host:Right.
Erik Antonsen:Like, this has to have and has to involve the most rigorous, systematic, and disciplined approaches to both, you know, no kidding understanding what is happening to the human body in this domain and how it changes — the mind, the behavioral health issues, our response to the radiation environment, galactic cosmic rays, potential solar particle events, our likelihood of medical conditions occurring. You know, the risk that we buy down from selecting the healthiest people in the world has been great for low-earth orbit, but you get diminishing returns when you get out to three years. These people are not superhuman.
Host:Right.
Erik Antonsen:They’re still human, right? And so what you’re really talking about when you say, “How do we approach this problem?” well, some of that probabilistic risk analysis and modeling is part of it, but we’re still building the tools for a lot of these things. We’re still building models, we’re still building experiments. The Human Research Program is still trying to make sure that they make investments in places where they get results that inform positively do we care about this, is it really important, or should we move on to the next problem? Because we got a long line of problems that we have to challenge, right?
Host:Yeah. And you kind of alluded to this before — and this is — I’m going to bounce into a topic, you know, thinking about we have so many questions that we need to answer, but we are investigating things right now. So let’s go into that. You know, what do we know? What do we know right? And there’s been instances like you said before — you kind of hinted at this in beginning — there’s been, you know, medical things happening you said on MIR. What were some of the things that were happening? And then what did we do to resolve them real-time?
Erik Antonsen:Yeah. So there’s — there’s a variety of different things. And this actually feeds how well we validate some of the modeling that we do to try to predict the future. Right? You remember that there was one episode where there was a fire on MIR. And one of the medical issues that comes out of that is smoke inhalation. All of a sudden you got people inhaling smoke — maybe haven’t gotten to their mask in time or things like that. And now you have this exposure potentially toxic exposure that’s also causing them to cough and to, you know, not be able to function. And you have to make a decision about hey, do we actually, like, get out of here, right? Even if you contain the fire, if you’ve got a crew member who is incapacitated because of the results of that fire because of burns or because of smoke inhalation or something like that or, you know, maybe that fire damaged something like the ammonia lines and all of a sudden off toxic exposure, right, you have to try decide what do we do about that in real time? There were — there was at least one case of a cosmonaut who had a cardiac dysrhythmia who was disorbited from it. And — and we’ve seen changes in heart rhythm as we’ve gone through the space program.
There have been astronauts that had atrial fibrillation. The question mark is, like, is this something that, you know, we need to not have somebody fly for? Or all of a sudden, you know, they never had this problem, and you get into spaceflight and maybe they have it there. We actually haven’t seen any of that in the AmErikan cohort, but there was one Russian who was deorbited for it. And then there’s that question of, like, if you follow that to its logical conclusion, all right, that sort of explains why we do the biological monitoring that we do — heart rate, that sort of stuff. You see in Apollo 13 and other movies they have these pads on and you got a signal sending down to the ground. Sometimes your problem is you may actually have too much information and information that you don’t know what to do with. So a lot of what we continue to learn as we go forward is do we really want to know this? Right? And what I mean by that is something we find things in clinical medicine on the ground that we call incidentalomas, right? You go and you scan somebody’s head because they — you know, they got in a car accident and you’re worried about it. And you don’t find any evidence of trauma, but you find something there that you’re not sure what to do with that wasn’t bothering them before.
Now that can set off a chain of events. Do we have to go look at that further? Do we have more specialists involved? Does somebody get poked and prodded? Do we start causing more problems than we solve because we saw this thing that we don’t know what the significance is? And that happens in terrestrial medicine all the time.
Host:Right.
Erik Antonsen:Now transplant that to the spaceflight environment where something happened. We measured something, we don’t know if this is a big problem or not. Are we going to do more harm than good to a crew member or to a team by chasing after it, or should we wait and see? Right? That’s a challenge. This is in the clinical world. In my job in emergency medicine I run into this a lot, right?
Host:Yeah.
Erik Antonsen:What’s the appropriate amount of concern that I should have for somebody who’s really healthy, highly functioning, not having any problems? And then there’s this thing, a CT scan or an ultrasound that was found, right?
Host:Yeah. And it sound like a judgment call based on the physician on the ground. But the problem is now you’re not getting as much data as we go further away, correct?
Erik Antonsen:And so you now find that line, which is where the science and the art of doing these things meets, right? I mean, in clinical medicine today, right, we don’t know everything. There’s still lots — huge — amounts of clinical trials going on that inform us and update us on what the best things to do are for our patients. It’s no different in spaceflight. As we go longer and learn more, we incorporate the corporate memory that we’ve had from the past and the things that we’re learning there to update what we’re doing. But at some point you’re operating in a domain where you don’t have a huge amount of evidence to influence what you do. And this is where flight surgeons and operational support have to make judgment calls. And that is that line between science and art of how you actually do these things. And that’s the beautiful thing about this job is that you live in that domain where we’re constantly pushing the boundaries of what we know and how we understand it in the larger system of what we’re doing. And you get to build the science to help inform the art.
Host:So I’m guess we have a lot of — a lot of practice with the International Space Station now?
Erik Antonsen:So you’ve got 18 years of people being up there.
Host:Right.
Erik Antonsen:That — it’s interesting. When people bring up, “Hey I have this concern,” right? Radiation is going to turn bacteria into these horrible, mutant, virulent beasts, and people are going to get sicker than they’ve ever gotten before. And then you look at the Space Station, and yeah, we swab the surfaces and we measure this stuff. And we have scientists here look at samples and all that sort of stuff. And yeah, there’s some stuff growing up there that, you know, you don’t want to hear about. But at the same time in 18 years, you’ve never really had somebody get sick from those particular bacteria or those things growing. You’re not having this epidemic of astronauts, you know, all of a sudden, you know, ending up incapacitated because there’s some fungus or some mold growing in the corner, right? And so it’s that — that’s part of what informs the judgment, right, is hey, how do square the science and the things that we’re learning about the way genetics, and bacteria, and viruses get modified in this new environment, and our own body’s immune systems changes, and our T-cells drop over time when we’re in microgravity and low-earth orbit?
And what are the consequences of that? And then you look up at the clinical level and you say, “Well, nobody’s really getting that sick, so how much do I have to care?” That’s great, six months. We’ve got a pretty good establishment of that.
Host:Yeah.
Erik Antonsen:I’m not too worried about it. Three years with all three of those things that we were talking about earlier no longer being available. How comfortable do we feel extending that sort of experience-based judgment calls and the art side of this out into that domain? And that’s what helps us guide where we put our research investments in the science is to help inform that for these longer, and longer, and longer duration things that we’re looking to do.
Host:Which is a lot of what we’re doing on the Space Station is learning what we learn here, we get to kind of package and then take out. Obviously there’s going to be things we’re going to have to learn along the way. But it’s a pretty good model, especially operationally whenever we’re doing things day-to-day. I did want to circle back, though, to you said there’s stuff growing on the Space Station, you know, all the time. But 18 years, not really a concern. What’s growing, and how come medically we’re okay?
Erik Antonsen:Well, this is, like, if you think about your house on Earth, right?
Host:Yeah.
Erik Antonsen:And you can certainly find websites and companies that want to go clean up all the fungus and the mold in your house. And maybe at some point you get to a point where that stuff actually starts to bother the people in your house or you have people who start having allergic reactions, but, you know, it’s really not a different thing than there. There’s fungus, there’s bacteria. There’s a variety of bacteria that we bring on our skin everywhere we go. Right? And some of these are the most common bacterias that we worry about in terms of infections, right? Staphylococcus aureus is a naturally occurring colonizing species on your skin — we all have it.
Host:Eww.
Erik Antonsen:I know, I’m sorry. Staphylococcus, right, when you think about strep throat, these things live on our skin, right? They don’t really actually cause problems for us until they get into someplace where they’re not supposed to be, like, for example, if somebody gets a cut and all of a sudden, like, bacteria from the skin is now down in the bloodstream or in the subcutaneous tissue and all of a sudden, you know, maybe you get an infection there. If you’re really healthy, you probably don’t. In terrestrial medicine the places where we see this is people with diabetes and with suppressed immune systems and stuff like that, right? That’s where we really worry about it in terrestrial medicine. But hey, when we’ve measured the T-cells in our own immune system in flight, we’ve seen some changes there. We see the T-cells decreasing over time in the microgravity environment. So where is that point at which hey, we’re kind of approaching an immune suppressed status and we might need to worry about this more? In the case of these six-month missions, we haven’t reached that point, which makes us feel good, right? That’s — that’s helpful. But at a year or two years as we stretch that out, do the T-cells keep dropping or do they threshold and plateau someplace?
If think threshold and plateau someplace, maybe it won’t be a problem with all the bacteria we brought up. Maybe our body can handle it because it normally can. But I don’t know if they plateau or if it keeps going down and then you’re going to have a problem in two and a half years right at that point you’re on your way back from Mars but you still have long enough to go that you could get really sick and not be able to do much about it. And by the way, all those medicines you brought with you? If we look at the formulary on the International Space Station right now, about 16% of those medications that are on the International Space Station could within the labeled expiration dates actually make a trip out to Mars and back.
Host:That’s good to know.
Erik Antonsen:So on the way back, if you still have three months to go, most of your medicines, they may not work if we were just using what we had on the Space Station today.
Host:So what do we do to extend the life?
Erik Antonsen:That’s a good question [Laughs]. That’s one of the areas that when I was working for exploration medical capabilities, we laid out a pharmacy research plan to try to address just that stuff, right?
Host:Right.
Erik Antonsen:Some medications seem to be affected by the spaceflight environment. We’ve left stuff up there for about 880 days and we’ve seen increased degradation rates in what we call the API’s — the active pharmaceutical ingredients — compared to stuff that’s on the ground, right, controls that we look at. And it’s hard to suss out why. Maybe some of it’s radiation, maybe some of it’s the environment, some other things. But what we’re trying to get heads around is are there biochemical categories of medications that make more sense to rely on because other ones break down faster in that environment? Some things that are happening in the pharmaceutical industry in terms of, you know, adding additives to pharmaceutical makeups can actually extend those expiration dates; can we take advantage of those sort of things? Do we try to make medicines that instead of having to take twice or three times a day for ten days for your antibiotic course, you take once, right? NASA doesn’t do that stuff, but we look to the pharmaceutical industries and the advances that they take to try and pull intelligently the things that are going to extend our pharmacy and make it more functional over the timeframes we’re talking about.
Host:Yeah. Now, this — this kind of goes back to you talking about, you know, what happens after six months? Does it plateau or does the immune functionality continue to decrease? What knows? But my assumption would be if it does, if we do have to worry about possibly go — decreasing — now maybe you’re taking more medication, now maybe you’re being extra careful where if you do get a cut, oh, you want to patch that up immediately because you don’t want anything getting in. Now you’re talking about using more resources.
Erik Antonsen:And having to bring more to be able to enable that.
Host:Right.
Erik Antonsen:Which we don’t have a lot of volume for.
Host:Right.
Erik Antonsen:It’s this — this ultimate backpack game, right?
Host:Yeah.
Erik Antonsen:How do you build up the best understanding of what changes are going to happen and being impactful? So you only bring the things that really matter. Like, right now we have a defibrillator up on the Space Station, and it’s an ongoing source of discussion, right? You’re familiar with the defibrillator like in the airport? You put it on, you shock somebody’s heart if their heart were to stop.
Host:Clear, yeah.
Erik Antonsen:Clear, bzzt [Laughs].
Host:Right.
Erik Antonsen:The whole — the whole point of that sort of thing is that when the heart enters certain electrical rhythms that don’t pump blood, you stun it and reset it, right? But what you’re really talking about, the underlying problem before that and after that is what’s wrong with this person that their heart actually entered that? And most of the things that would lead to that are stuff we screen for and get out of the way in the astronaut corps, right? So we don’t really expect them to be in a position where they’re probably going to need that. The likelihood of it happening is extremely low. And so if you’re really up against the wall in terms of the volume, does it make sense to bring that, right?
Host:Right.
Erik Antonsen:I don’t know because it’s a really, really, really low likelihood event, but it’s really high consequences if it happens. But part of the way we answer that is by looking at all right, what else comes with that? If you actually shock somebody, it doesn’t mean they’re automatically okay, right? This is not TV. [Laughs] It means that you’ve got a whole bunch of other work to do and a whole bunch of other resources to bring to bear to do resuscitation on somebody who’s really sick. And the odds of us being able to supply those sort of things in this small volume and space is really, really small, right? So now you start asking the question, “Is that a risk we’re willing to take?” And it’s a challenge.
Host:Yeah. Because now you think about oh man, but what if we do need it, right? But you’re saying — you’re pretty confident based on we’ve flown so many times and we’ve gotten, you know — if you’re thinking back to Fred Hayes, back to that time, we were kind of figuring out spaceflight. That was the whole point of Mercury, and Gemini, and Apollo is to keep going further and kind of figure it out along the way. Now we’ve done it a lot. We kind of know what we need to do before a spaceflight to make that spaceflight successful medically too. So yeah, maybe you can kind of take it away and feel confident learning from these operations.
Erik Antonsen:To paraphrase Frank Borman when he was sitting in front of Congress, right, the places that we’re going to fail after this much time are the places where we have a failure of imagination, right? It’s the things that we didn’t know about that are going to come and bite us. And there’s going to be enough of those. So we have to intelligently plan for the things that we do know about. If something is really, really low likelihood, we probably need to be making room for things that are much more high likelihood that will help to us make sure that we don’t let those small problems, the little cuts to the skin, the infection in the urine, the other things like that grow into the big problems that all of a sudden we’re never going to be able to provide the resources to handle if it reaches something like a sepsis level.
Host:Do you find that, you know, meeting with other doctors and other people in your field, getting together, you’re still coming up with more questions that needs to be answered?
Erik Antonsen:I would say that all good science lead to more questions.
[ Laughter ] That’s just the reality of the world in which we live, right? As soon as you start nailing down something in the evidence base, you immediately have the question of wait, but what if this happens or what if our assumptions about this weren’t correct? How does that change what we would do? And that’s an ongoing conversation and question that we have with the flight surgeons, and the research doctors, and the research scientists, and the immunologists, and the toxicologists, and the systems engineers? Like, this is what the ongoing conversation is that occurs between the people doing a lot of the research in these areas and the people who are doing operations right now for the programs that we have set up. I mean, SS is the most big and visible of them.
Host:Sure.
Erik Antonsen:But there’s other things that are happening — the commercial crew programs and how we interface with those guys, Orion’s coming up, and then soon to be Gateway. Like, these are all going to have unique challenges. And everybody that’s got experience to bring to bear, they have a piece of the puzzle for figuring out how to do it safely and how to do it right. Right? And then there’s also people who are working in field that we haven’t had to pull on yet that are going to have other pieces of the puzzle. So how to do it safely and how to do it right?
Host:Now I know, I mean, just personally working with large groups, you get a lot of different input and diversity of thought, which is good. But then you have everyone providing so much input that you can’t agree on anything.
Erik Antonsen:At some point you got to make a decision [Laughs]. How does that happen?
Host:That was going to be my question. How do you — I mean, you do want as much information as possible. Because that’s how you’re going to be successful. But then how do you — how do you know which things to sacrifice? You know, you’re already talking about a defibrillator. How do you know which things to sacrifice to come to an agreement on this is the most important elements of what’s going to make a mission successful?
Erik Antonsen:Yeah, so part of this question is really wrapped in what at NASA or who at NASA makes decisions, right, after they have looked across all this stuff? So there’s a couple of different places. I work with the Human Health and Performance directorate. My job right now is assistant director for humans systems risk management. And one of those parts of that job is to chair the human systems risk board. I started that a couple months ago, it’s actually a new job for me.
Host:Oh, cool.
Erik Antonsen:But the purpose of the board is to look across all the risks that we have to try to assess the evidence base to understand, hey, how big of a problem is this, how well do we understand what as going on, how well do we expect to know what’s going on in a few years, you know, and how do we prioritize where we should put our investments? And that board is a wide group of people who look at these problems from a bunch of different angles. And they come together and no kidding, no everybody goes away happy all the time. But it’s one of those hey, we got to have a transparent and open discussion about what the puts and the takes are when we’re looking at these programs and how we’re funding our research going to the future. And so that board actually flows out of the Health and Medical Technical Authority. There’s three technical authorities at NASA that were founded after the Columbia accident. When they were looking at what were the pressures that teams that were looking at the risks and the challenges and the science of what they were doing — what pressures were they facing just because the agency had goals and they were sometimes pushing on people to meet them, right?
Host:Sure.
Erik Antonsen:So what they did was they established three independent reporting lines. People who had no dog in the fight for actually getting and meeting program schedules. One of those is an engineering technical authority. One of them is a safety and mission assurance one. And the third one is a Health and Medical Technical Authority. And it derives its power from the chief medical officer and headquarters at NASA. But the responsibility of that group is look at the risks, look at the evidence base, look across all of these problems and start prioritizing. Right? And start making some of those hard decisions about if we’re going to make standards that we hold future programs to and requirements about whether or not you’re going to have a defibrillator or something else, right, that those — those things have an open and vigorous debate about the benefits and the costs potentially, the risks of including this and not including that.
Host:Yeah.
Erik Antonsen:And so we’re always working to try to improve how much information we bring to bear, how we actually communicate, right? It’s very easy for technical people in these fields to speak with jargon and to potentially leave other experts who are, you know, as accomplished in completely different fields sitting there, thinking, like, they’re idiots because I don’t understand what this person is saying.
Host:Right.
Erik Antonsen:So you’re talking when we come to these boards, what we’re talking about is bringing expertise, and engineering, and spacecraft, and systems engineering together with medical doctors, together with life scientists. And all of them are speaking their own languages, all right? It’s a big challenge. So this past year, the former chief medical officer — guy named Rich Williams from NASA — actually commissioned a book called the Rosetta Stone. It’s a handbook for trying to get life scientists, fit medical doctors, and engineers to understand each other’s perspective and the language they speak in. Because we’re always trying to figure out how do you take people who have a huge amount of insight and understanding in this field over here and get them to understand what the problems are in a different field? That communication is a massive challenge.
Host:Absolutely. Oh, I want to check that out, too. Because that would be probably good across the board just communicating with folks that maybe speak a different language than you.
Erik Antonsen:Yeah, we just published that one a couple months ago.
Host:Nice. Well, focusing on that, now you said you’re focusing on human systems risk management, but you also are actively practicing emergency medicine. So with that comes a certain perspective when it comes to what you bring to the table. So what are some of the things that you’ve been bringing to the table recently?
Erik Antonsen:So I maintain practice in emergency medicine up at Ben Taub. I’m professor at Baylor. And NASA actually buys my services from Baylor as a professor. The — my perspective is informed by what do I do in emergency medicine in my practice today? And maybe even more so, what would I rather have been done so that somebody didn’t have to show up in the emergency room, right, the preventative aspect of care?
Host:Captain Hindsight.
Erik Antonsen:I get a lot of opportunities to say, “Man, it would have been great if you would have just done this or known that or, you know, and the system had this sort of thing plugged in.”
Host:Right.
Erik Antonsen:And that’s part of it. The other half of my background is I was a PhD engineer, aerospace engineer in propulsion. I used to do that for the Air Force Research Laboratory. So I spent a lot of time both as a medical doctor kind of dealing with the realities of the sickest people that we see in Houston — Ben Taub is a level one trauma center. It’s a lot of indigenous, immigrant, uninsured population that we deal with there. So people who have not had the primary and preventive care we would like to see, and therefore they end up in emergency rooms more often than not. And then I also have spent time as an engineer for spaceflight, looking at how propulsion systems mesh with the larger vehicle systems. And so when I look at the problem of human system risk, I’m looking at it from the what’s the right answer on the medical side hopefully to prevent the problems that I see and deal with in my practice? But how do you make that jive with the realities of the engineering life cycle of designing a vehicle? Right? One of the biggest oversights that the physicians have in the flight surgeon cadre who have never been exposed to an engineering design life cycle is they don’t even know what the words mean, right?
Host:[Laughs] Goes over my head.
Erik Antonsen:These spacecraft, when you’re starting to build a spacecraft, right, you have different phases that engineers all understand — prephase A, phase A, phase B. You don’t actually fly one until you get to phase E. And prephase A can start a decade before you actually build this thing. Right?
Host:Wow.
Erik Antonsen:So when you’re actually designing and creating the requirements that a Boeing, or the NASA engineers, or SpaceX, or somebody’s going to go build this spaceflight do, you kind of need to know what you need to get it into the mix at least five years and sometimes longer ahead of time.
Host:Wow.
Erik Antonsen:Now, contrast that with what happens in the medical world in technology development, right? All of a sudden we have this explosion of innovation in the medical world. What we’re learning and how we use things like iPhones, which didn’t exist when I was in grad school, right, or even in medical school, like, the technology that we are able to bring to bear on understanding the human system just for terrestrial medicine right now is changing so rapidly that if I said, “I want to use this thing in five years for my medical practice,” I would be doing my patients in five years a severe disservice.
Host:Right [Laughs].
Erik Antonsen:Right?
Host:You can’t do it.
Erik Antonsen:So now think about the Space Station, right? It’s 2018, we’ve been having people up there since 2000. The first module went up in 1998. The design freezes that occurred for what was going to be included on this vehicle in the year 2018 happened probably three to five years before 1998, right? I got my first cell phone of any kind in 1998 [Laughs], right? The ways in which we handle data and expect things from our technology are completely different today than they were then, right? We don’t have automatic means of capturing a lot of information up on the Space Station and the things that we do have are fixes we’ve made after the fact. So when we talk about designing something like the Gateway vehicle or, like, what’s going to take us to Mars and you’re trying to figure out what the right things to include are today, knowing that that mission may not happen for five to ten years, but if you don’t actually put placeholders and things in there, then the engineers aren’t going to actually keep volume and mass for your stuff, right?
And this is the problem. What we have on the Space Station today in terms of a medical system is good. We have an environmental health monitoring system. We have a health maintenance system, which is some medical kits with equipment and supplies and medicines. And we have a countermeasure system, which involves exercise equipment that we’ve changed over time, right? None of the data from any of those things is connected. Right now if you wanted to know for your, like, fitness how well you’re doing on keeping up with your stuff, you’d use your Apple Watch, or your MyFitnessPal on your phone, or something to track your job in the park. And you could, like, see how you’re doing over time, right?
Host:Yeah.
Erik Antonsen:None of that stuff was designed into the Space Station. But it’s an expectation on the data that we have for today in the world that we operate with that we’re at least going to have that sort of interoperability with the things that we send on a crew to Mars. But remember, NASA’s been operating and optimizing a system for the last 18 years that hasn’t needed that. So it’s actually a shift, a big shift in the way we think about the way we do business in low-earth orbit. We have put up some things like apps with iPhones and iPads — not iPhones but iPads. And sometimes we’ve learned things that were surprising. Like, the certificates for the Apple iPad and the apps that they have, they don’t — since they don’t have a direct connection to the Cloud, all of a sudden your iPad’s going to stop working after a certain amount of time.
Host:Oh.
Erik Antonsen:Yeah. So now you got to accommodate in the networking that you do for the vehicle. And we still have problems with it. We’ve ran into it for the last several years. It’s those type of small problems that we learn in a systems engineering sense and in a data management sense in the Space Station today that we need to make sure don’t happen on the way to Mars. Right? So we’re learning in every aspect. It’s not just how the human body changes but even how we do data, how we set up our networks, how all this stuff talks to each other. And when we get into that place where we all of a sudden no longer have any real-time communications and you need to put that ultrasound on somebody and go look at their appendix or their kidney or something, and you don’t have somebody to guide you and tell you which way to point the probe, you better have included a learning module that shows them how and where to look and how to interpret the images.
Host:Yeah. So being conscious of your time, I’m just going to ask you one more thing: If you had to take something — just based on what we’ve discussed today — and let’s say we have a long-term presence on the moon, some folks that are practicing some of these things that we need to explore further out into the solar system, Mars being one of the destinations, what are some of the things that you are looking forward to trying on the moon?
Erik Antonsen:So there’s a giant list.
[ Laughter ] Part of it is actually managing the data that we have and learning how to do that with a different ground support model than we currently have today. Because those are the first steps of what’s going to enable us to change from the ISS paradigm and the everything readily available paradigm over to something that’s going to be appropriate to going to Mars. That’s one way that we learn to do the mix of monitoring the human system that we worry about, along with making sure that we can be supportive in whatever ways we can be. Another thing is we don’t have a dose response curve for gravity and what happens with the human body. Right? Those T-cells that I told you about declining?
Host:Yeah.
Erik Antonsen:I don’t know if that’s isolation, stress, radiation, microgravity, right? You put somebody on the moon, all of a sudden you have a data point at one-sixth gravity, right? We don’t know the neurovestibular changes that happen. We don’t know how long they’re going to last when you go into one-sixth gravity. We don’t know how well the body’s going to accommodate in one-sixth gravity compared to microgravity, right? Or three-eighths at Mars, right? So part of spending time on the surface of the moon from the perspective of the human and how we change is starting to get another data point somewhere between no gravity and the three-eighths gravity that we expect on Mars. And right now all we’ve got is 1G and zero, right? So that’s a really amazing opportunity to start collecting data in a partial gravity environment and start building that dose response curve to what happens to the whole accommodation, right? You’ve heard of the sands problem, sometimes called VIP, where they have the eyeball changes, and some astronauts have had changes in their vision and need to wear glasses and that sort of thing?
How’s that going to change when you put partial loading back on the body? When you actually have the fluids in the body pulled back down again. But maybe not that much, right? It’s a whole new set point for adaptation that we’re not going to understand that until we spend some time there doing it, right? We didn’t have enough chance in the ’70s when we were at the moon to really start kind of gauging those questions.
Host:Right, they were camping trips.
Erik Antonsen:We’ve got basic functionality, right? Can we do this? Can you walk around? What happens if you fall over, right? And also we learned that astronauts would hurt themselves in creative ways [Laughs]. You know, when we do our modeling for the loads that people experience and we’re worried about hey, are these guys to break their bones because of the changes in their bone density and stuff like that? Most of the modeling of loads that we would expect to be applied says no, it’s too low of a load in these gravitational fields. And yet one of the astronauts, you know, managed to go out there, get a piece of equipment stuck in the ground, and then trying to get it out, stuck his shoulder up underneath it and really hurt himself pushing up against it, right? It’s those sort of things that oh, I didn’t know that person was going to do that. I probably should be aware of that and take that into concern or into my calculations for what I provide, right? [Laughs] It could be anything from, like, potentially fracturing a bone to pulling a muscle, to just having a bruise. We don’t know, but it sort of reminds us that when we think we have solutions and we think we have answers, humans have a wonderful way of surprise us.
Host:Yeah. It’s those extra data points that are really going to be — really going to help us out. But then just learning along the way, what questions do we still need to ask?
Erik Antonsen:Yeah. Right now we’re comfortable with the evacuation times we have from the Space Station. What happens when we’re living in that domain where it takes three days? How do we change the way we view medicine? How do we change the way we view prevention? How do we change the way that we support our crews as we get farther and farther away from Earth? As that distance increases, the question marks just multiple. So that’s one more set of data points and ways in which we can start to understand the real impact of that hazard, which is distance from Earth.
Host:I can’t wait to find out.
Erik Antonsen:Me, too.
Host:Erik, thanks for coming on the podcast today and sharing your perspective on what it takes to go far, far away.
Erik Antonsen:I appreciate you having me. Thank you.
[ Music ]
Host:Hey, thanks for sticking around. So today we talked with Dr. Erik Antonsen. We talked about being far from Earth, the distance from Earth, and all the challenges that come with it. This is part of our series of the five hazards of human space flight. We’ve had several podcast episodes so far — two down, I guess this is our third, and two more to go. We are actually partnering with the Human Research Program to do this series. So they have a video series and animations that are paired with each of these episodes. You can go to NASA.gov/hrp to see those videos and the content that’s supplemented with these five hazards and the three that we’ve done so far. For the International Space Station, you can go to NASA.gov/iss. A lot of the research we talked about today is on board the International Space Station. So you can go to that website to find out some of the research going on there. Otherwise you can follow us on social media. It’s Facebook, Twitter, and Instagram for the International Space Station or the NASA Johnson Space Center accounts. Go to those, whatever platform is your favorite, and use the hashtag #AskNASA to submit an idea for the show.
Just make sure to mention it’s for Houston, We Have a Podcast and we might make a whole episode out of it. So this podcast was recorded on June 28th, 2018. Thanks to Alex Perryman, Pat Ryan, Bill Stafford, Nell Whiting, Bill Polaski, Judy Hayes, Isidro Reyna, Mel Whiting, and Thalia Patrinos. Thanks again to Erik Antonsen for coming on the show. We’ll be back next week with the fourth of the five hazards of human space flight, discussing altered gravity fields. See you then.