From Earth orbit to the Moon and Mars, explore the world of human spaceflight with NASA each week on the official podcast of the Johnson Space Center in Houston, Texas. Listen to in-depth conversations with the astronauts, scientists and engineers who make it possible.
On Episode 249, Dr. Scott Dulchavsky and Dr. Dan Siegal reflect on research aboard the International Space Station that has improved ultrasound training and access worldwide. This episode was recorded on June 2, 2022.

Transcript
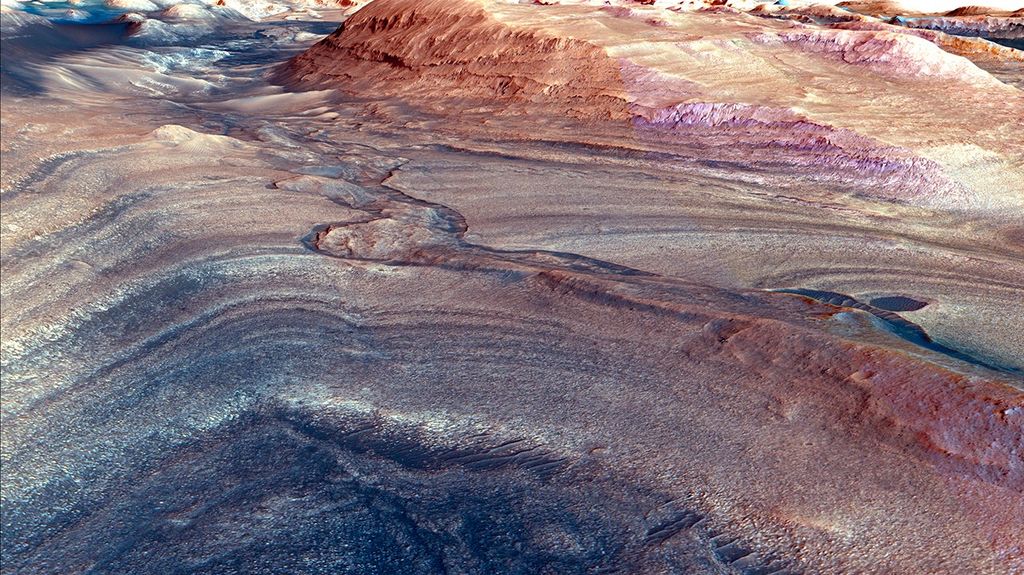
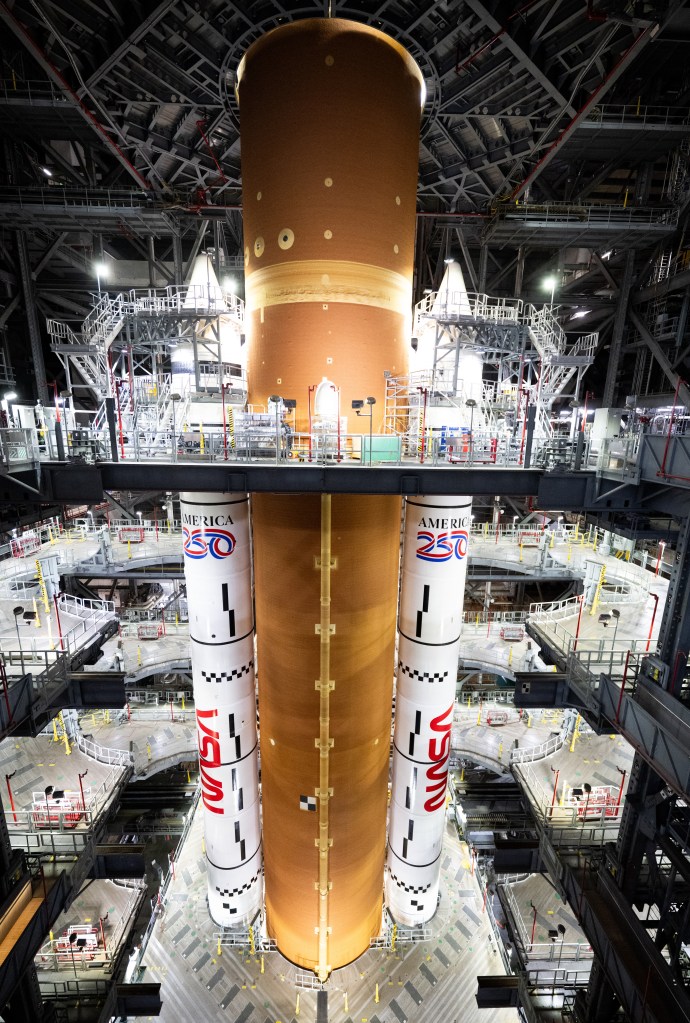
Gary Jordan (Host): Houston, we have a podcast! Welcome to the official podcast of the NASA Johnson Space Center, Episode 249, “Ultrasounds Anywhere.” I’m Gary Jordan and I’ll be your host today. On this podcast we bring in the experts, scientists, engineers, and astronauts all to let you know what’s going on in the world of human spaceflight. If you live in a bigger city, chances are you live close to a hospital that is at least a drivable distance. It’s not always the case, though, particularly in more remote areas. And it’s definitely not the case for astronauts living in space. With long-duration missions, having remote access to medical professionals is a must. A project on the space station called Advanced Diagnostic Ultrasound in Microgravity, or ADUM, was created to see how to potentially diagnose medical conditions and injuries in space through ultrasounds. On the way to Mars, there’s really no turning around to find a convenient hospital for medical examinations, so astronauts will need to be able to help their fellow crewmates on the go from millions of miles away. ADUM successfully demonstrated this capability of remote ultrasound on the space station, but what if we could broaden the scope and use the same capability to conduct remote ultrasounds here on Earth? This eventually created a foundation for WINFOCUS, the World Interactive Network Focused On Critical Ultrasound and the world leading scientific network for ultrasounds. On this episode, we’re joined by Dr. Scott Dulchavsky, principal investigator for ADUM and surgeon in chief and chairman at Henry Ford Health in Detroit, Michigan; and Dr. Daniel Siegal, musculoskeletal radiologist, also at Henry Ford Health. Both doctors will be discussing how these projects not only impact long-term spaceflight on the International Space Station, the Moon, and eventually Mars, but how it can and has impacted the people here on Earth. With that, let’s get right into it. Enjoy.
[Music]
Host: Scott and Dan, thanks so much for coming on Houston We Have a Podcast today.
Scott Dulchavsky: Great, great to be here.
Daniel Siegal: Thanks so much for having us. Wonderful to be here.
Host: Very good. We’re going to get into ultrasounds and how we, and how we took that into space and then around the world. But to, to get a sense of who we’re talking to when it comes to, you know, that this, this ADUM investigation, and then, and then what’s grown from it, let’s first understand sort of, who you guys are. Scott, if you’ll, if you’ll start with some of the things you’re working on and what led you to, to where you are today and your involvement with, with ADUM and, and with NASA?
Scott Dulchavsky: Sure. I’m a surgeon at heart and, I’m up here at Henry Ford in Detroit where I’m the surgeon in chief, but if you go back 30 years a medical school classmate of mine wanted to and became an astronaut, and he introduced me to all of the unique challenges in a pre-International Space Station era there were on diagnosing problems that might occur in our astronauts when they exit the planet for a number of years. Ultrasound at that time was a novel technique outside of radiology, and we were only beginning to use it in very limited scenarios for the diagnosis of patients after trauma. So we were just getting these new machines in our hands and trying to figure out what to do with them, and I thought there might be some applicability in the shuttle and then space station because these machines are getting smaller, more portable, more easy to use and more powerful.
Host: Excellent. Excellent. Now, what, what is, what is it about, you know, at the time, what was a, a newer technology, what was so fascinating about ultrasounds that could reveal something medically to you, give you information that you needed? What, what was great about ultrasounds?
Scott Dulchavsky: You know, my partner on the call is a, is a radiologist and he’s been extensively trained in, in ultrasound. In fact, it’s Dan’s specialty, and he can talk about that in a minute. And they have always used it for classic indications. Probably many of the people listening today have had an ultrasound “congratulations your child will be a boy.” Or my gosh, you’ve got ultra, you’ve got gallstones or perhaps you have an abdominal aneurysm in that. But we had such unique things that were occurring on shuttle and space station where we’re trying to develop additional diagnostic capabilities. And then you had all these challenges. We were not planning an x-ray machine or a CAT (computerized axial tomography) scan or an MRI (magnetic resonance imaging), so how would you diagnose things like a collapsed lung or a broken bone or things like that, absent these capabilities? So we started to think about, OK, how do you train somebody really quickly, not a doctor, generally, to use a pretty advanced technology — Dan has spent years getting the skills together to get images — and then can you use them in novel locations in that, such as diagnosing lung problems, never been done before. So we proposed this to NASA and they thought it was quite interesting, hence this ADUM, Advanced Diagnostic Ultrasound in Microgravity, initial experiments that we started almost two decades ago, and have continued now for all of that time in, in a broad expansion. One of the things I’m really proud of is we showed not just that these very talented astronauts and cosmonauts can actually do these exams, but that they work. And when we started looking at, could you diagnose a lung problem with this – yes; in fact, so well that now that’s come back to the planet and it’s a standard done every day. So if we are worried about a collapsed lung in my emergency room, more likely than not you are going to get an ultrasound examination, very quickly done, cheap — it can be nearly free — no radiation, and provide you immediate results that we’d have to wait for a chest x-ray before. Now that’s a standard everywhere, and that, that initially started from these very small investigations off of our planet on NASA facilities, funded by NASA, and that, that’s impacted terrestrial medicine. And that can be done on a mountaintop, we’ve done it on Mount Everest, been done in sub-Saharan Africa, military conflicts, and all that. It’s just a wonderful story.
Host: And that’s the story we’re really going to get into, but, but, but first let’s, let’s take a pit stop to Dan. Dan, you mentioned, Dan, your specialty is radiology. This is, this your focus and of course, you saw the, some of this potential that Scott was alluding to. Can you tell me how you got into your field and how you got looped into, into the world with NASA to, to really kick off some of the things that Scott was talking about?
Daniel Siegal: Sure thing. I guess the, the easiest way to start is to say that at my heart, I am a technologist. When I was an undergraduate I studied computer science and thought that I was going to go off and become a software designer, software developer, before I was inspired by a mentor who happened to be a surgeon, just like Scott, and inspired me to take my passion for technology and apply it as a clinician. The, the, the way he really inspired me was to show that the easiest path to integrate the technology and the clinical side of things was to do it from a clinical perspective. And I loved imaging at the time; I loved the idea that you can look at a picture of a, of a, of a human being and be able to understand what’s going on inside the body from a physiological or pathological sense, and use that information to make a decision about a treatment or an intervention that can really help them in a very immediate way. There’s just such an, an evolution that has happened with imaging even since I went into the field about 20 years ago, where the image quality has improved, the technology has advanced, and we’re now able to do things with handheld devices that was just not even imaginable before this, this miniaturization of technology has advanced. And I’m particularly excited about ultrasound because it does a couple things that other imaging technologies don’t do. If you think about a CAT scan or an MRI, they’re really taking a snapshot in time. But what ultrasound can do is get a real time view of things that move inside the body. You can actually see the beating heart. You can actually see a baby move, and when you look at my specialty, which is actually the musculoskeletal system — bones, joints, tendons, and the like — it’s an incredibly valuable tool for looking at injuries, because you can see when things move correctly, and you can also see things that don’t move correctly. So when you’re looking for broken bone, torn muscle, torn tendon, those kinds of things, you can see that almost immediately. And one of the other great things about ultrasound is there’s really no contraindication, unlike a CAT scan which gives off radiation or an MRI which has a very strong magnetic field and then can have all kinds of problems with that, anyone can get an ultrasound at any time. So it’s, it’s really a, a great tool to have in the hands of any clinician. And, and one of the great things that I’ve seen evolve over the last 20 years is that we’ve, as medicine in general has adopted that, and we’re starting to see ultrasound used by more and more clinicians in more and more different areas, and it really truly is portable: it translates up into space, it translates out into remote and rural parts of Earth, and it’s a tool that with the right kind of guidance and the right kind of training can really be effective in the hands of almost anybody. So really, really love ultrasound and love to see how it’s being used in new and interesting ways all the time.
Host: Excellent. You’re both alluding to this, this fantastic growth in the technology and the applications of ultrasound, and both of you have been in this field for, for a very long time. Let’s, let’s take it back towards the beginning. Dan, we, we’ll stick with you for just a second. It seems like earlier, earlier in your career you, you, there was this, this technology, this ultrasound technology, and I’m sure that you, you guys were both thinking about what are the potential applications here? This, this technology is, is incredible. And I wanted to kind of pick your brain on earlier in your career, when you were thinking about ultrasound as a technology, to how that led to, let’s try to do something in space?
Daniel Siegal: Well, the first thing that I would point to there is that these machines used to be the size of refrigerators. They were very big, very expensive, and the screens on them were, were microscopic. It’s amazing we were able to make the diagnoses that we could, but what I think it showed is the potential for, as we’ve seen with most things in, in computerization and, and, and technology like this, we knew it would get smaller. We knew it would get better. We knew that eventually it would grow to the form factor that it is right now, where it almost the size where it can fit into your pocket, plug into a handheld screen, and give you the ability to, you know, with a little bit of a battery power, take it anywhere, including up into space. And the, the second thing I would point to is ultrasound has a reputation for being somewhat difficult. It’s easy for anybody to pick up a probe, but sometimes it can be a little bit challenging to train them to put it down on the body in the right place, get the right picture of the organ or structure that they’re looking at, and know that what they’re looking at is normal or abnormal. And very fine movements of your hand on the probe can have a pretty dramatic change in what the image looked like. So one of the things that I’ve really been focused on, and if I would go back a while back to sort of think about how I thought that this should evolve, is a lot needs to be built into training people to use ultrasound effectively. You don’t need to be an expert in order to get perfect images, but you do need a basic level of understanding in order to get good-enough images. And so we’ve put a ton of work into, into the education and training programs that teach, not just clinicians, but also, novice users, students, astronauts, others that may not have ever held an ultrasound before, how to guide themselves to get really, good quality images. And one of the things we’re starting to even see now is software that can run on the ultrasound machine itself that can provide automated guidance. Really, really exciting technology, potentially gives anyone, even an untrained user, the capability to use a probe anywhere in the world, or anywhere in the, even up in space, to get these images and make a diagnosis from them.
Host: Oh, excellent. Now, Scott, when you, when we first came to you, you talked about the applications on the shuttle and on the space station, with some of the, when, when Dan is going over the progression of the technology and how portable it became, I wonder how, how you guys ended up working together on this investigation called ADUM, and maybe even before, and, and after ADUM as well. But sounds like, you know, you’ve spent a lot of time working on this technology, and then, and then these, these capabilities of training non-medical doctors, so, so in many cases, astronauts, how to use the device. So, so can you talk about the genesis of the, of the, some of your efforts to, to, to start applying this technology in space?
Scott Dulchavsky: Yeah. As Dan suggested, it’s been a, an iterative process, part of it was involved with the technology advances. So it’s quite difficult to fly something the size of a refrigerator; it’s impossible to make that portable to take out into a sub-Saharan Africa or India or something like that. There’s a cost prohibitions that are, you know, less relevant for a space program but completely relevant when you’re trying to democratize this in a, in an underserved region. So we first had to slowly modify and wait for the technology to catch up. And as Dan suggested that has been explosive in that there are, there are hundreds of companies that are continually making this technology more user-friendly, more powerful, better, better image quality, and things, things like that. I think the, the partnership and, you know, you’re missing a really important component in this, so I’m a sort of surgeon that understands some of the unique challenges within space, Dan is a radiologist who is an expert in ultrasound that dwarfs my capabilities in that, but the third is the user, in getting that user interface. It is not going to be Dan, whose got hundreds of thousands of hours on probe; me who has tens of thousands of hours; I might have somebody that’s got tens of minutes and that, so that user is critically important. So I think what we did really well was talk to the crew, who were going to be, OK, what is the best way you learn things? And that’s what ADUM was all about, is to get those just-in-time training programs in place that made sense for an astronaut crew, but interestingly make sense for a medical student or for a nurse midwife or for a policeman or for an army corpsman, in that to be able to quickly get these skills. So that, that’s what ADUM was all about is this sort of this tripartite partnership that would allow us to go, oh, OK, this is how you might train somebody. And that’s what’s been durable for the 20-some years with some improvements in animation and things like that. The second part of this was, OK, great, we can get a picture; would that picture be appropriate for use in the various scenarios that might occur in space, such as the lung condition that I mentioned earlier, or problems with the bones, if you hit something up there, problems with spine, we did months of work with the astronauts in orbit on some of the spinal challenges that they’re having. That again, happened back here on the Earth, that would mandate a multi-thousand dollar MRI evaluation. Most recently, working on some of the ocular problems that we see in our long-duration crews in that, and then looking even more forward to exploration-class spaceflight in the air, changes in the fluids that are appropriate, fluid balance in astronauts a long time off the planet, which are also appropriate for heart failure patients here back on Earth; looking at changes with lunar dust that might be diet-detectable with ultrasound that would, again, coming back here to look at people that are exposed industrially to small particles here in that. And then finally, and maybe even the most exciting that we might talk about later, is looking way future-wise about how can we non-invasively, as Dan suggested – just a little goo on a probe on your skin, and that doesn’t hurt, it doesn’t really cost much — could we use that to monitor things more longer term, like diabetes? Whether you have diabetes, how well you’re doing; whether you will get diabetes? And that it’s a really, a novel technology that powers are almost, almost limitless. I hate to say it’s like a “Star Trek” tricorder, but it, it’s sort of the closest thing we have right now.
Host: So if I were to sort of summarize and, and maybe Dan, I’ll, I’ll toss this to you, sort of summarize, Scott, some of his thoughts here when it comes to working in space, it sounds like, sounds like there’s a, there’s a component here of evolution and maybe, maybe talking about ADUM is really just more of a snapshot where the technology improves and they become more user-friendly, and you want to continue to use the latest and greatest technologies, so, so you can keep exploring new ways to, to refine the training program and, and use the technologies in space for monitoring in space but then it sounds like it’s, it’s translated to a lot of things on, on the ground as where, as well. Is that, is that a fair summarization that there’s this, there’s this evolution with the, with the training and with your efforts when it comes to ultrasounds that maybe follows the, the technology progression?
Daniel Siegal: Yeah, no, that’s, that’s certainly accurate. You know, one of the things I would say about ultrasound, and Scott was starting to allude to this, is one of its greatest strength is its versatility. You can use ultrasound to diagnose an almost unlimited number of conditions in the body, with very little restriction and very little limitation. And you can do so in real time, like we were mentioning before. And that’s just a capability that you don’t have with pretty much any other imaging technique that we see. Certainly not anything else with the portability, and low-cost and availability that ultrasound has now become. And that has been a evolution over the last 20, 30 years. And you know, that, that becomes really important because one of the things Scott was just saying is that, you know, we can anticipate some of the common issues that are going to come up in space, whether it’s fluid shifts, changes in the bone, that sort of thing. But there’s a lot of unanticipated things that come, that come up, and particularly when we think, you know, even more exploration or next generation type stuff, whether it’s to the Moon or Mars or beyond, there needs to be a very versatile diagnostic tool, kind of like a tricorder. We’re not quite that far along yet, but it, it certainly gives us the capabilities to put a diagnostic tool in the hand of someone that can deal with unexpected issues. Whether that’s appendicitis, gallstones, trauma, injuries, those can all be really well evaluated with ultrasound. And so that ability to deal with unexpected issues is something that there is really nothing else that we have right now that, you know, ultrasound is really the best suited for.
Host:Interesting. I want to, I want to stick to space for just for just a moment, and, and Scott go back to you for a second because, you know, one of the things you mentioned is, is that through this capability and making, making the ultrasounds user-friendly, I’m sure, you know, they may, they may or may not have been operating on the, on the, you know, kind of on the own, or maybe, maybe with you guys, but if you can talk about when it comes to actually working with the astronauts to refine some of these techniques, can you talk about some of the things that you did and then some of the things that you learned through this demonstration of working with astronauts in orbit?
Scott Dulchavsky: That’s a wonderful question because it’s, everybody’s experience in space is so limited, right? We, it’s, it’s mere hundreds of people that have spent any time off our, off our planet. And so, we had some initial assumptions, some of which were blown out of the water, others which were realized in, in, in spades in that. And I think that we trialed so many of these technologies, first on the ground then we modified them and used them in NASA microgravity research facilities, the, the parabolic flight program, in that sort of look at the usability of the ultrasound in zero gravity. Some of the, how do you hold — ultrasound requires you to take the probe and push it on something, and anybody who’s spent any time in lower gravity knows when you push on something you get pushed away from something, so how you restrain yourself is critically important. And astronauts got really clever really quick on how to do that without fatiguing themselves, without moving the machine or the patient or themselves away from things. So that was really kind of fun. And I think one of the things that they continually tell us about is things that were highly-value added — their time is very critical — in that, can we cut down on some of the training in certain areas that they saw it was redundant or not, not necessary; alternatively, areas that they thought they needed additional expertise in, either through training or, or through hands-on experiences in that; some technology upgrades that they, that they suggested to us, some educational upgrades that they suggested to us. But I’ll tell you, the real eye-opening thing to me was, and this was almost to a man and woman of the individuals who were, as Dan suggested, they were a little frightened about ultrasound early on because it — the images on the screen do not look like a heart, they look like a bunch of gray lines that are moving oddly in that, so, but most of them having either a military or a, a piloting background, are really good with hand-eye coordination with, and with spatial recognition, in that they really quickly figured out pattern recognition. So we would say, don’t worry about all this other stuff: this one, this is, little area that would really, make that area really sharp by moving the probe around. Ah, got it. And so, we developed a nomenclature of how we could talk together, communicate really effectively. So that communication, we call it remote expert guidance: basically, the astronauts are being our robots when we’re in real time — that will not occur on Mars with a 15-minute delay — but how we could really effectively communicate. And that is now durable. That’s how we do it across the planet when we do remote guidance on this. And the second one is, I under-anticipated how well that they could do that, absent us in that. So we, we would have real-time sessions where there was some fair amount of handholding required, and towards the end of their expeditions, boy, I was superfluous in that. And so much so that not only would they get the image, but they would start to make diagnostic impressions on that image. Hence our next grant, which was the catalog grant that just went, it, it was ADUM on steroids, so it was a head to toe assessment in that, and not only was it that you could get an image in that but then you could compare the image you got to a catalog of either normal or disease images. So if you are on Mars and you are a minimum of a 15-minute time delay phone call away from somebody, probably longer, that you could at least gone, ha, this looks like that, and they could start to make plans for that. They’d obviously have expert oversight at some point in that. But it was quite remarkable to me that they were able to acquire this when I was sort of, haughtily as a doctor who spent so many hours doing this, going, “man, you picked that up pretty quick.” And that sort of empowers me, and I hope our teams, to go, you know, this has been in the realm of very experienced doctors in the past, and probably people with a lot less training and skill in this can be pretty darn good in this technique.
Host: And that I think leads perfectly, Dan, I’m going to toss to you because I’d like to switch gears here for a little bit. Having, having this capability done in space, what I’d like to do is build from there and sort of take those lessons and, and Scott’s listing some wonderful ones, right, about some of the things that we learned, and how this, this experiment has translated, I think into one of the more recognizable, in our terms, benefits for humanity. In the way that we, we tried to solve a problem in space and, and it became something that can be approached in sort of our everyday lives and reaching folks around the world. Can you talk about that progression from, from space to, to the applications worldwide?
Daniel Siegal: Absolutely. And, and I think the perfect example of that is remote guidance. It’s this idea that, whether you’re, you’re ten miles away or thousands of miles away, to be able to see on a screen what a user remotely is imaging and provide them feedback in real time has been an incredibly powerful tool to enable us to essentially reach more people. You can have an expert available to provide guidance, to provide feedback, to perhaps even help make a diagnosis if it’s something new or an unusual condition, and you don’t need to have the level of expertise that Scott was saying, maybe we thought that we needed to have out in rural areas, in underserved areas, in areas with difficult terrain or otherwise hard to get to. We can now acquire those images — don’t need to necessarily send the absolute expert out there — but have the capability when needed, on demand, to get online and provide that teleguidance, that’s been incredibly powerful. And, and that’s something we’re actually using here in Detroit to do something as simple as go out to patients’ homes and check in on them, provide imaging when needed of things like their lungs and heart, and have now real, quantitative and qualitative information about how they’re doing, and be able to better make decisions about can they still recover at home or do they need to come back to the hospital. And that’s enabling us to really put the technology to use in a way that is impactful for people, because we want to keep people healthy, we want to keep them out of the hospital, and having the ability to see this, even remotely, and provide that feedback when appropriate has been, has been really beneficial.
Host: I think what’s, what’s, what’s particularly special is just how expansive this is, what you’re talking about. It’s certainly being applied in, in Detroit, but I understand there’s been this effort to, to create almost a network of folks using ultrasounds. I believe it’s called WINFOCUS and I, this is, and I think there’s been some evolution even from WINFOCUS, but can you, can you tell us a little bit about that and how the, this idea that, that you guys have been working on, and of course, our practicing now in Detroit, going in, you know, having this incredible access where folks at home can, you know, can be receiving treatment and, and insight, but how, how it truly has expanded and how truly grand it is now?
Daniel Siegal: Sure. I mean, I can give you the, the beginnings of that but Scott is really the, knows a whole lot more about how this got started. I’m really the recipient of the, the energy and expertise that has been poured into this to create this group. But what it does is it really recognizes that ultrasound is a very diverse and very democratic technology because it can be used by so many different experts for so many different reasons. Me as a radiologist and a musculoskeletal radiologist, I’m using it day in day out to diagnose tears in muscles, ligaments, tendons, other injuries, that sort of thing. So that’s a very different application than say an OBGYN or a surgeon or a internal medicine doctor who is seeing someone in their clinic or out in their home or out in some remote area. So the idea that you can bring together a network of experts to talk about, to research and better understand how to standardize the use and applicability of a technology like this, is really important, because otherwise you could see how it would go off in a hundred different directions, and potentially, disrupt or inhibit the ability of it to be used, in, in, in positive ways. Bringing together all that expertise collectively and having a continuous discussion really seems to be the right way to understand the value of it, not just for one individual specialty but as a whole.
Host: Excellent. And, and, and Scott, Dan mentioned that you can certainly expand upon that being much closer to this, to this WINFOCUS, and then of course, I, the evolution of that?
Scott Dulchavsky: Yeah, so we, we developed this wonderful tool for use on, in space, and the tool that we got — we, we did not develop an ultrasound machine, those are externally developed — what we did was take how to make a very complicated and lengthy training program a lot more efficient. And so we had this, it worked great at NASA, they continue to use the large components of this today at NASA. How do you get the word out? And so we started to look at partner organizations, or if not available, to form them. And WINFOCUS was, as the name says, world interactive network. So we wanted to get this out on a global basis. And so WINFOCUS is involved in individuals across our planet that are trying to take this new technology for the betterment of humankind in areas that were, never had these capabilities before. And so, we’ve worked with the United Nations on that, UNESCO (United Nations Educational, Scientific and Cultural Organization) and many other areas in that we’ve presented this in, in countless formats. And WINFOCUS is that organ that gets the word out, that does the training in that, now in 68 countries and tens of thousands of students, much like the American College of Surgeons. When we showed this technology to them, they went, “wow, that’s fantastic; let’s use that as the training platform for all surgeons.” Or medical schools, and they went, “my gosh, this is phenomenal.” And that, let’s now use this to train the, the next generation of individuals. What Dan is now doing is, almost the neglected people in this are the physicians, and so Dan is now working with different groups of physicians who previously only ordered ultrasounds are now starting to perform them. So internal medicine, family medicine, dermatology, people like that that can now have and utilize this really important technology to make medicine more efficient, more cost-effective and hopefully safer and more timely.
Host: Dan, this, this level of access and level of user-friendliness seems to be a huge component to this, to this incredible technology. And, and Scott described pitching this to other surgeons who reacted with, you know, a surprise and then amazement and, in its applicabilities. I wonder if you’ve received the same level of excitement when, when reaching out to others that have helped it to what it seems like continue to grow?
Daniel Siegal: Absolutely. We have wonderful colleagues in our surgery department, in our emergency medicine department, in our internal medicine department. It’s really gotten to the point where people recognize that a portable ultrasound has all of the power of a stethoscope in that it gives you the ability to not only listen but also look and see what’s going on in real time inside the body. So I wouldn’t be surprised if in five years or so, or possibly even sooner, we see most physicians starting out in medical school not having a stethoscope around their neck but having one of these portable ultrasound devices. And it even translates to what happens with patients. When I’m in a room scanning a patient and they see the actual images coming up on the screen in real time, documenting whatever their problem might be, they become more engaged as well. And so, it just goes to show that the power of seeing a picture right in front of you in real time is so much more valuable than anything we’ve really ever had before.
Host: Scott, I want to circle back on the surgeons. How you, you, you mentioned their level of excitement. I wonder from your perspective as a surgeon, a very experienced surgeon, what, what you find most useful and fascinating about this technology and about this access that’s getting you and many other surgeons in particular that, that, that particular focus of medicine, on board with, with this capability?
Scott Dulchavsky: Yeah. Surgeons are pretty impatient individuals and, in that we like immediacy of action; often we’re forced into that — in a trauma scenario, minutes, minutes, count in that, and having to wait for a diagnostic examination can be life-threatening in that. So I think I really appreciate the immediacy of information that it provides. Dan mentioned, but it deserves additional emphasis, that rather than a, it’s not a polaroid of what’s going on, it’s a movie camera. And so certain things you can only pick up when you can pick up motion in that: the way we diagnose a collapsed lung is watching the motion of the lung, and that can be lost sometimes in a singular chest x-ray or things like that. And then finally, I think having a tool that is, has such broad applicability in that you don’t have to have a hammer for this one and a nail driver for that thing and then the screwdriver for this, in that you have a single machine that you change some settings on and you can use it to look — is your bone broken, or do you have an infection in your, in a cavity in that, are you pregnant, do you have appendicitis in that, all with the same darn device. And that, that, oh, by the way, cost less than a couple thousand dollars now from $250,000 when we first started this and that. So I really appreciate that this technology, it can, is really at the forefront of how to be almost, you know, seeing into the human body in real time.
Host: Thinking about the evolution of this technology that’s, that’s been mentioned and, and just what we can look forward to, Scott, you alluded to things like monitoring diabetes or using the tricorder as a diag, diagnostic tool. It doesn’t seem like there’s any, any indication that the things are slowing down in this world, if anything, that the possibilities just, just continue to, to grow. I wonder, you know, what, what some of these tools are and, and how can they, how they can really help the people on Earth, that’s, that’s been started through some of the efforts in space, but then taking that, taking those technologies and, and thinking about space as well. I wonder, really what I’m getting at here is, how this can continue to grow, and how the possibilities continue to open up as we go through time?
Scott Dulchavsky: Yeah. I like to think that I’m sort of clever in that, but I’m always amazed when somebody comes up with some novel idea on how to use this I never thought of in that. So some colleagues said, hey, we’re having this problem, we worried about the, maybe the astronauts have increased pressures on their brains from something that’s going on in long-duration spaceflight, and that the astronauts were appropriately reluctant for us to put bolts in their head to monitor those; could you use ultrasound? And so, some colleagues said, maybe we can look at the back of the eye at some of the nerves and things like that, and darn it seems to work just famously about that? And so, we studied that, we proved that, and, and now it’s something that we’re using, you know, monthly on the space station and also, also terrestrially. And then I’d look at Dan and some of his basic colleagues that are starting to see some really interesting stuff in diabetes, so I’d like him to talk a little bit about this because he’s on the forefront of this.
Host: Oh, excellent. Yes, Dan, please.
Daniel Siegal: Yeah. So what, what Scott is alluding to is the ability to, I would describe look deeper into the images. What ultrasound and most imaging modalities were originally conceived as being able to do is to recognize abnormalities in the anatomy. What we’re realizing now with the ability to look at both the raw data and changes in the signal that come off of things like ultrasound at both an individual and an aggregate scale is there’s probably information in there that is not perceptible to the human eye, but when analyzed by an algorithm, a deep learning type of artificial intelligence algorithm, we’re starting to see patterns that may not have been, like Scott had said, even thought of or perceived. And we have the potential to see architectural changes in structure, like muscle or tendon, that are seen on images before they may even be detectable in blood tests. So diabetes is just one of those areas we’re exploring right now. We think we’ll have the ability to non-invasively detect things like that, and many other things, potentially giving us a predictive capability from these images that could keep people healthy, both on Earth and up in space, in addition to the already impressive capabilities that we have with ultrasound to diagnose things after they’ve happened. So that is particularly exciting. And that’s where I, I, I’m just so fortunate that I have this background in, in computer science to be able to understand and, and think about how do we apply these computational techniques to real world clinical problems. And it, there’s just such an opportunity to help a huge number of people, again both on Earth and looking at what we can do as we start to explore space.
Host: Yeah. And I, and I wanted to sort of circle back on that with you, Dan is, is there’s, there’s certainly a lot of possibilities here on Earth. And I wonder if, if, you have a similar level of excitement for, for the possibilities in space as well? I know we’re returning to the Moon, and we’re going to remain in low-Earth orbit; I wonder if as these technologies progress if, if there’s, you know, there’s ways that we can continue to explore these technologies and these capabilities as, as we send humans to some of these, some of these locations. Even thinking about Mars, too, which was mentioned as having a certain delay, but, but really capturing this idea of, of humans in space.
Daniel Siegal: Oh, without a doubt, without a doubt. We want to continue to push the envelope and, and really truly, there’s no better way to do that with, with folks like NASA and astronauts going up, both into space, to the Moon, to Mars, beyond. It’s a really unique opportunity. There’s truly nothing quite like that environment on Earth. And there’s such a need to have a technology, an imaging tool, that is both diagnostic and potentially predictive about some of the things that could go wrong when you’re looking at a months or years-long journey or longer. You really need to have some of those capabilities. And so I’m excited as some of these tools get smaller and smaller — we’re even thinking about making them wearable, which could provide real time information about what’s going on inside the body…could be really interesting as we look at those longer and longer spaceflights, zero gravity changes, all those kinds of things.
Host: Very interesting stuff. Let me, let me toss to each of you, Scott, you first, and, and then to Dan: I want to make sure we did this topic justice, reviewing some of the things that we’ve done in space and, and the applications to a lot of what has, seems like rapid progress over the decades in, on Earth, but I wanted to toss to each of you to make sure that, that we covered most of the things that we were hoping to cover. Scott, we’ll start with you.
Scott Dulchavsky: Yeah, I guess we haven’t fully explored what NASA’s involvement has in fact been with this. So yeah, we had a, an operational problem, we needed a diagnostic tool and we needed to have it small and portable and usable for astronaut and cosmonaut crews, and I think that we initially started and we did that, but the pressure from NASA about the, the educational constraints, you only have a limited amount of time with astronauts, my gosh it’s got to be a small device, it has to be user-friendly, it can’t have a lot of power requirements and things like that — really, really forced us to think differently about this problem. Absent those constraints imposed by NASA, I don’t know if we’d be where we, where we are today with this technology.
Host: Excellent. Excellent. And Dan, we’ll end with you. The same question, making sure that we did this justice, anything we left off that we really want to re-emphasize?
Daniel Siegal: No, I think we’ve covered it all, especially with, with what Scott just said about how important the contributions of the, the men and women who have gone up into space, and really put the, the hours in to prove this out has enabled us to do great things back on Earth. And I think that, that translation, that, that will continue to bear fruit in the future.
Host: Excellent. This is certainly one of the, I think more — one of the more popular topics here at NASA when it comes to what we do in space and, and how it applies to, to, to the betterment of humanity here on Earth. And, and this is I think one of the, one of our favorite ones. And I think what’s really exciting talking to the both of you today is that we’re not done; that, that this, there’s, there’s much more to do. So, so to Scott and to Dan, thank you both for taking the time out of your busy schedules to come on Houston We Have a Podcast and share all of the great work that’s been done in space and on the ground and, and all of the great work that you both do. Thank you very much.
Scott Dulchavsky: Our pleasure.
Daniel Siegal: Thank you.
[Music]
Host: Hey, thanks for sticking around. It was a pleasure talking with Dr. Scott Dulchavsky and Dr. Dan Siegal today to learn more about ultrasounds that have been conducted in space and really around the world, and what has been made possible through some of the efforts of NASA. It was really a pleasure to have them on. You can check out NASA.gov/iss for the latest going on in the International Space Station; of course there are ultrasounds still being conducted to this day. So you can check out some of the research objectives that are ongoing. We’re one of many NASA podcasts across the whole agency, and you can find us all at NASA.gov/podcasts, including us. And you can listen to any of our episodes in no particular order. If you want to talk to us, we’re on the NASA Johnson Space Center pages of Facebook, Twitter, and Instagram. Just use the hashtag #AskNASA on your favorite platform to submit an idea for the show and just make sure to mention it’s for us at Houston We Have a Podcast. This episode was recorded on June 2, 2022. Thanks to Alex Perryman, Pat Ryan, Heidi Lavelle, Belinda Pulido, and Jaden Jennings. And of course, thanks again to Scott and Dan for taking the time to come on the show. Give us a rating and feedback on whatever platform you’re listening to us on and tell us what you think of our podcast. We’ll be back next week.