From Earth orbit to the Moon and Mars, explore the world of human spaceflight with NASA each week on the official podcast of the Johnson Space Center in Houston, Texas. Listen to in-depth conversations with the astronauts, scientists and engineers who make it possible.
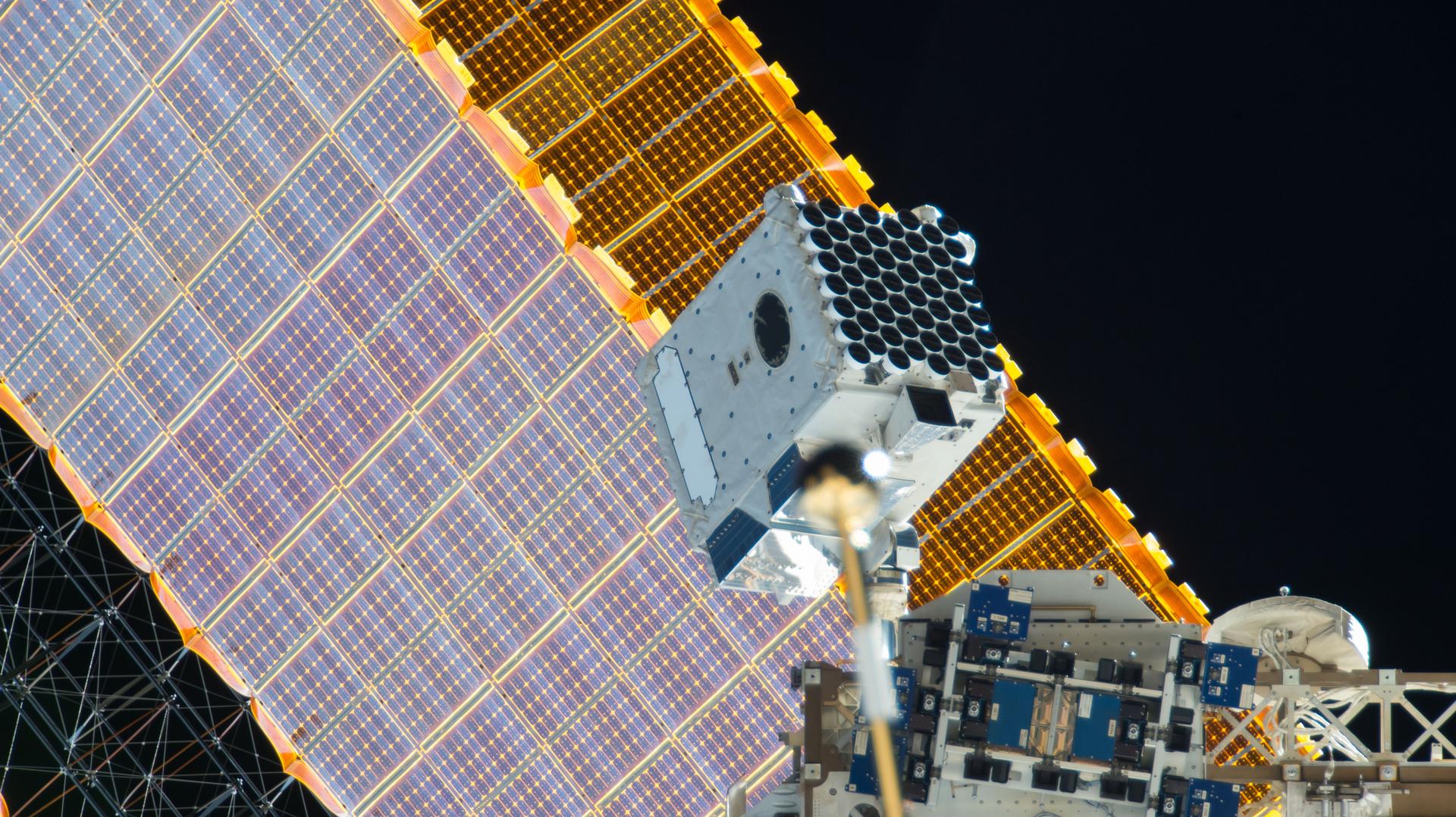
On Episode 291, co-principal investigator for a neuroscience experiment launching to the space station on Northrop Grumman CRS-19 cargo mission walks us through the goals of the experiment and how it might benefit patients back on Earth. This episode was recorded on April 17, 2023.

Transcript
Gary Jordan (Host): Houston, we have a podcast! Welcome to the official podcast of the NASA Johnson Space Center, Episode 291, “Improving Precision Neuroscience.” I’m Gary Jordan, I’ll be your host today. On this podcast, we bring in the experts, scientists, engineers, and astronauts, all to let you know what’s going on in the world of human spaceflight and more. We talk about microgravity experiments on this podcast quite a bit. Removing gravity from the equation is an intriguing thing for scientists and researchers and can offer new and unique perspectives into research. And particularly for cell cultures, microgravity offers a shift in perspective to three dimensions, and that’s what’s needed for this experiment that is about to launch to the station on the Northrop Grumman CRS-19 cargo mission. Scientists believe that this new perspective can offer insights into how microgravity can be used as a long-term platform to improve modeling of human neurological diseases and drug testing. It’s not an easy subject to dissect, but luckily, we have Shane Hegarty, chief scientific officer, and co-founder of AXONIS Therapeutics Incorporated, calling in from Boston, Massachusetts to help us break it down. He is the co-principal investigator on an experiment about to take place aboard the International Space Station that is looking into this very idea. All right, let’s go ahead and get started. Enjoy.
[Music]
Host: Shane Hegarty, thank you so much for coming on Houston We Have a Podcast.
Shane Hagerty: It’s an absolute’s pleasure. I appreciate the invitation. Very excited to discuss more about AXONIS Therapeutics and our project on the ISS NL (International Space Station National Laboratory).

Host: Yeah. And it’s very complicated, so I am absolutely trusting you to help us to navigate through this precision neuroscience. This is well beyond my expertise, and, and I think it’s, it’s a very interesting sort of field to pursue, but it’s, I mean, when I think about ways to explore science and, and, you know, I, I, I get sort of intimidated by something so comp-, so complex, and I wonder, how you got to where you are? What inspired you to pursue this sort of complex field?
Shane Hagerty: Well, you know, this has been a passion of mine for many years now, and I think I may, may, we may share some similarities in how we approach this topic. You know, I, I always need to simplify things for myself in order to understand them. And that, you know, usually leads to curiosity, leads to me digging into details, processing information, integrating, you know, multiple sources of information and just try to understand it for myself so I don’t embarrass myself. And that’s, you know, that’s something I’ll try to do today as well. So I’ve always been thinking about what do we know about the brain? What do we know about neurological disorders? What don’t we know? Why don’t we know these things? How are we going to study them? What tools do we have at our disposal? How do we try to solve the lower hanging fruit of problems? And then, you know, it obviously gets complicated quickly, but you have to start somewhere. So, you know, the, the, even the goal of this project is to improve precision neuroscience modeling, and test, one of our, one of our therapeutics. Again, it, it’s all about pushing the boundaries of what we know already. And, you know, in this case, we get to leverage things that you can’t do on Earth, which is microgravity conditions and, and I look forward to getting into that. But also, you know, we can also take a step back and talk about neuroscience in general, what my company, AXONIS Therapeutics is aiming to do in this space and how we got to where we are today.
Host: And Shane, I want to do all of that, right? I definitely want to, I think what we’re going to talk about mainly is we’re going to lead up to talking about this experiment on, on board ISS, why microgravity is such an interesting place for this idea of modeling, right? But, but I do want to, to set some context. Let’s start there. Let’s start about, you know, like there, I think there’s different ways that you can approach modeling. You know, there’s probably different companies that you could have gone to, but you decided to be a co-founder of, of this company. Can you talk about the inspiration of kind of going off on your own and saying, “you know what, I think I, I think I want to start, I think I want to build something from the ground up.”
Shane Hagerty: You know, just to be very clear, this is a, a team effort. It was a group of people…
Host: Sure.
Shane Hagerty:…who shared this vision. You know, we’re standing on the shoulders of many people’s work, and it’s a, you know, at this time, at this time point, a whole operation, you know, built on initially discoveries from Boston Children’s Hospital and my Harvard Medical School where I joined, you know, back in 2017 to try to do something different to what I’d been doing before. And the, the motivation to, to spin out our discoveries from academia into this biotech was just a simple question of we’ve made these exciting discoveries, how quickly can we see if they’re going to help patients? And that’s the quickest way to do it through biotech rather than in an academic setting where you, you dig into details, you know, you’re, you, you move a little bit more slowly. Here, with the right people, with the right support, we want to make it therapeutic, and we want to test it in the patients, you know, in a very safe and effective way as quickly as possible. And that excited me, and that’s, you know, why we, we took that, that leap. But it was based on, you know, as I said, many, many years of work, primarily from my professor in Boston Children’s Hospital in Harvard Medical School, professor Zhigang He. You know, the company’s really founded around his discoveries. And, and right now, my job really is just to separate those from a pre-clinical, you know, breakthrough, scientific discovery into an actual medicine.
Host: The — absolutely fascinating speed seems to be one of the important drivers here, and I think that’s really important, right? Is, is your, like, you know, you know, you, you mentioned speed as a primary driver. Really, what I think what you’re, the motivation here is you want to help people out. You want to develop drugs as quickly as possible. You, there, there are people that, that need these sorts of remedies and, and your, what you’re trying to do is get them, get them their help as fast as possible.
Shane Hagerty: That’s correct. And, you know, there’s a lot of room for improvement in medications for neurological disorder. It’s a very difficult area to develop drugs for. Hard to study the brain. It’s, it’s, it can be fairly inaccessible. You know, it’s not like you, you know, you can take a, a blood sample, for example. So it can, it can be complicated, but there’s a lot of exciting new developments, new models, things we’re working on. And I think in this century, we see huge progress in how we treat these disorders.

Host: That is very exciting to hear. And, but I want to understand exactly what are those challenges, right? You said it’s, it’s, it can be hard for neurological diseases.
Shane Hagerty: Yeah.
Host: What are the challenges? What, what exactly are, are the ways that you could develop drug, that you can test drugs, develop treatments, and what, what is the hard part? What are the barriers?
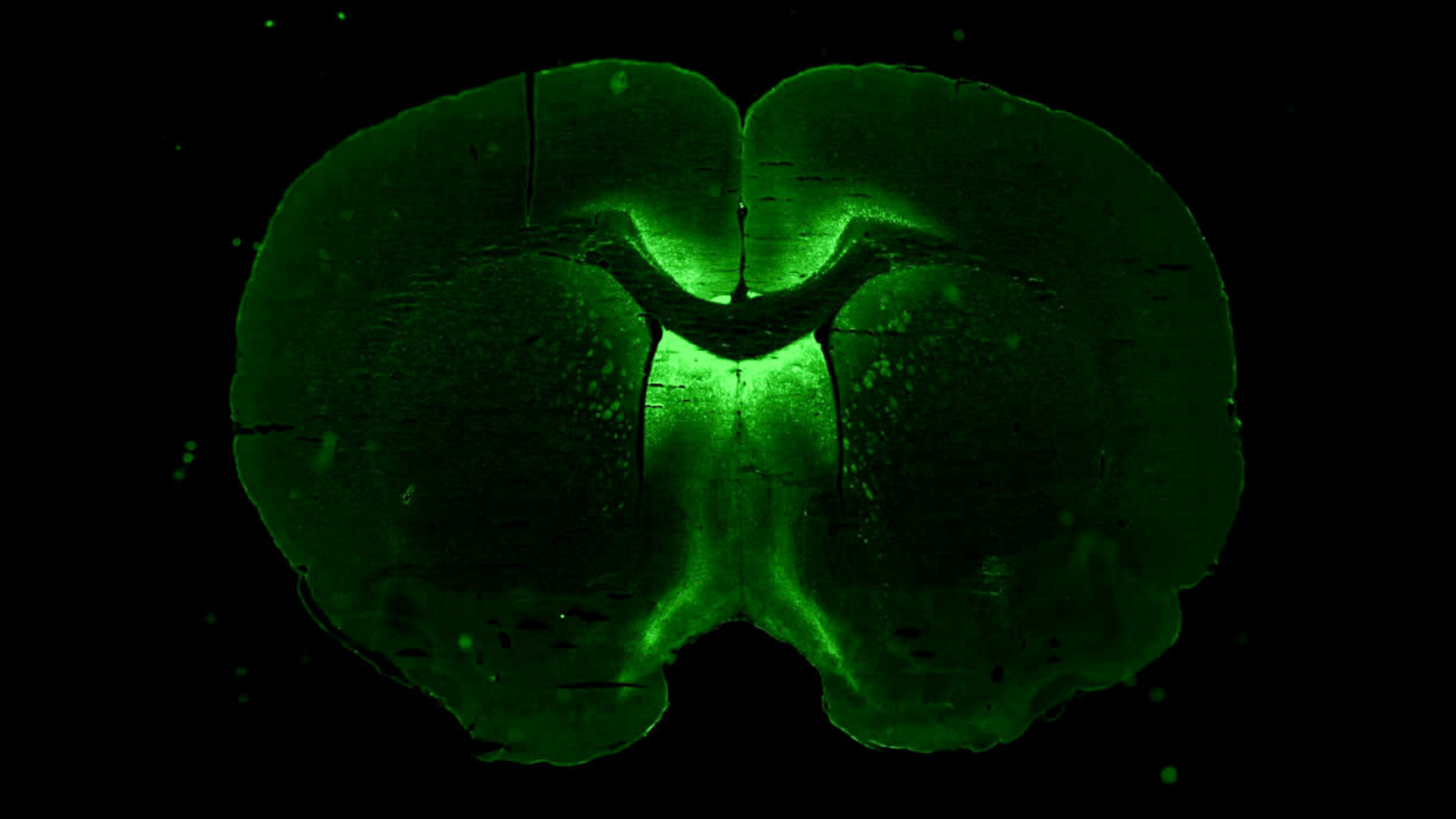
Shane Hagerty: You know, the, the reason there’s, you know, been difficulties in developing therapeutics for the nervous system is it’s a very difficult thing to study in humans. You know, we do have some imaging technologies. We can take samples, bio-fluid samples from the cerebral spinal fluid or the blood, or we can look maybe at postmortem tissue to try to figure out what are these pathologies. But it’s very hard to take, you know, biopsies, for example, which, you know, is possible in epilepsy, but more difficult in other, other indications. So what that means is, if we can’t model the disorder, it’s hard to study, it’s also hard to then test the therapeutic. The model has to come before you test the therapeutics. So that’s the part where we can be limited in, in some cases. And at AXONIS Therapeutics, the reason we are able to make progress and, and spin out some new discoveries that people haven’t thought about before, was to do a very ambitious modeling and screening workflow. This is because our professor Zhigang He back in Harvard Medical School and Boston Children’s Hospital, he was a geneticist, turned neuroscientist. So he was very much in favor of doing unbiased forward genetic screens where you have a biological question and then you do the screening and let the data speak for itself. What is the most important gene manipulation that controls this phenomenon or that phenomenon? And these were the discoveries that led to AXONIS many years ago. And the first, he did multiple screens. The first one was to determine what genes regulate axon regeneration. And for many years it was thought that neurons, once they’re injured, they can’t regenerate because it’s the external environment around the neuron blocks that process. But what [professor] Zhigang proved was, if you manipulate an endogenous gene, you can cause the neuron to regenerate its axon. And that was very exciting discovery, but it didn’t stop there. And when I joined the lab in 2017, there were two ambitious screens going on at, at the same time. One that we devised together. a large crisper screen using AAV (Adeno-associated virus) gene therapies in, in a mouse model. And the other screen was a model of spinal cord injury where we were trying to reactivate the damaged tissue in the spinal cord to see if we could get to restore a movement in this model. And we’re working in-vivo, which is quite rare to do screens in-vivo. They’re very labor intensive. You know, usually, people would screen in a cell culture in-vitro and a disc. We did that in the animal models because we can all appreciate that the central nervous system is very complex. There are neurons wired in complicated wiring systems. Each part of the brain and spinal cord have region-specific functions. There are multiple different cell types co-functioning. So we have diff-, we have, you know, millions of neuron subtypes. We have astrocytes, we have microglia, we have oligodendrocytes. They’re all cohabiting and interacting and supporting each other’s function locally. And then, we have other organ systems, you know, the blood, the blood brain barrier. We have inflammatory cells. They’re all impacting the central nervous systems. So if you go to this, you lose that whole body comp, you know, complex interactions, which are very important in pathology. So that’s why we took the trouble of doing in-vivo screens. And from those screens is made the discoveries of targets, therapeutic targets. These are proteins or genes, depending on how you want to treat the disorder, that when you manipulate their function, you can give a benefit in the model and hopefully in the clinic. So we studied a couple of different pathologies, as I said, which studied ways to prevent neurons degenerating. We studied ways to, when a neuron is injured, cause it to regenerate its, its connection. And the third thing we studied was, when a tissue’s been damaged and the neurons aren’t firing the way they should, can we get them to rebalance their activity? Because what happens when the activity isn’t balanced? You have things like, spasticity, which is uncontrolled movements. You have hypersensitivity to touch, which is basically leading to neuropathic pain. And you also have lack of movements. So usually you could coordinate a movement, you lose that ability to control your movements. So these are the types of things we were studying in Zhigang’s Lab through these large screens. They were very difficult. Many people involved. What we found were breakthrough discoveries. And those are now what we translate through AXONIS into new medicines. So the, you know, why did we want to create a new model and leverage microgravity conditions? Well, I just spoke about the benefits of doing in-vivo screens in animal models. We wanted the whole body, wanted the CNS (Central Nervous System), the different parts. I went over that. But what were we missing there? We were missing the human biology. We were still studying, you know, these are mammalian models. They’re as close as we can get, you know, in, in, within reason to studying pathophysiology of disorders and then testing new therapies. But we are missing the human biology angle. So in, you know, in, in recent years, there’s been a big breakthrough in modeling human disorders. And that’s the ability to take a skin cell from a patient, reprogram it into a stem cell, then take that stem cell known as an induced pluripotent stem cell, and differentiate it into your cell type of interest. In this case of neuroscience that will be a neuron or a glia. And then study the human pathology in that model. And that’s very exciting. That’s what we’re building on here with our ISS NL project. And that’s been a huge advent for neuroscience drug discovery and precision neuroscience. We can, you know, model individual patient disorders. We can differentiate the cell types of interest and study those. And we can also grow these induced pluripotent stem cells into organoids over time that we capitulate human brain in a 3D system with multiple cell types interacting. However, what is a limitation with that is, on the ground, it can take a long time to get these induced pluripotent stem cells to form these 3D organoids that resemble the brain. It also means that once you decide to differentiate the induced pluripotent stem cell, you have to decide what it’s going to become. That you can’t make multiple different things at once. You either have a protocol to develop organized, you have a protocol to develop a particular cell type, and then you just have, you know, a kind of a monoculture in some cases. So what are we trying to solve on the ISS NL? Now, we’re, we’re trying to explore whether we can take these cells and have them 3D self-assembled in microgravity conditions, which has been proven for other cell types. And we want to see that when we do that, do we get this 3D assembloid of neurons and glia? And if we can do that, then we want to see if we can use your precision therapeutics to target only the neurons and not the glia. So that’s kind of an overview of our goal on the ISS NL. And the reason we’re doing, as I said, is to study the human pathology, try to rapidly develop a 3D model of, of the brain. And if we can prove that we can take any cell from any patient, differentiate the multiple different types of cells that we want, and then assemble the different categories together in space, because as I said, on orbit, I mean, on the ground, you have to choose one differentiation kind of route. If we have multiple different cell types, and then 3D self-assemble this mixture on orbit, then we can have a, a more complicated model, multiple different cell types, multiple different neurons. It’s a couple of different types of glia and, and have them temped together in that 3D space, which is important for recapitulate in the, the brain, especially in, in one, in the case for our project, we want to see, follow the tropism of our gene therapy. So if you just have a single layer of a cells, you lose that, lose that information. So this is, these are the types of questions we’re trying to answer through this project.
Host: Very complicated. I mean, if I, if I had to break it down, basically what you’re saying is, you know, you have the, the, the company that you are, that you’re with allows you to have this aggressive schedule of modeling, testing, modeling, testing, modeling, testing, right? And…
Shane Hagerty: Correct.
Host:…but, what’s the limitations of, of, of the way that you have to model is you can only do sort of these, you can only target one, almost section at a time when it comes to a neurological disease. And neurological disorders can, can target, you know, different parts of the body. So you’re looking for something more complex. You’re looking for a model that’s more complex and more representative of what it would be like for to test a drug in a human. And so, you are coming up with some ideas that microgravity, that in microgravity that will allow you to create, and I know they’re three-dimensional, but is, and I guess what, what I’m, what I’m interpreting, and maybe you already said this, was, they are also more complex and therefore, more, more robust whenever you actually start testing some of these, some of these, some of the drugs and, you have more confidence, your hypothesis at least, is that you can maybe have more confidence in that model because it’s more representative of the complexities of the human body.
Shane Hagerty: Exactly. And the, the, there’s another advantage to this as well. I mentioned the organoid. These are brilliant models. But they can take many months to grow into organoids and become mature to study, you know, your question of interest…
Host: Yeah.
Shane Hagerty:…because in microgravity conditions, you take your cell types and they should, you know, based on other, other reports and other cell types, rapidly self-assemble into a 3D structure. So you kind of, you know, that’s saving a lot of time on the organoid, you know, timeline. At the same time, when you grow the organoid, again, it’s going to be a very select type of differentiation process where you can’t get every cell type you’re interested in. And another progression of the technology of, of induced pluripotent stem cells is directed differentiation. Before these protocols were very, very, they took a lot of time. You were changing, you’re, you were almost trying to come up with a recipe of reagents in the media, like the food that the cells are sitting in to make them to become a, a motor neuron or sensory neuron. You know, there was a, there was, it was very complicated. It took a lot of, a lot of time. But more recently, what we can do is genetically reprogram the induced pluripotent stem cell to rapidly differentiate them into a neuron subtype of interest. So that can be much quicker. But again, it’s, you, you, once you decide which cell type that induced pluripotent stem cell is going to be rapidly differentiated into, you know, you, once it’s differentiated, you, it won’t go back. It will be that cell type, but you’ll be missing the other cell types you’re interested in. So it becomes less complex. So the idea would be, you could make multiple different cell types of interests with these rapid differentiation protocols, then on orbit, leverage the microgravity conditions to self-assemble these multiple different cell types. Just like in the human brain, there, as I said, trillions of neurons, millions of different cell types. You want them, you want to recapitulate that. So the more complex the model is, we can look at the different cell types interacting with one another and try to make a better model than we’ve been able to do on Earth. And in that environment, ideally, as I said, 3D, you know, to, to, to mimic their, to allow the interactions of the axons of one another, microglia interplaying. If you, if we can also have them interact with those astrocytes and human neurons, which is what we’re planning for our first pro-, protocol. And then test your therapeutics. So there’s, there’s two, two parts of the project. One is, is this a useful model? Do we have the human brain assembloid on, in, on the ISS NL? And if we do, can we study different patient phenotypes by using their cell types and differentiating them into the neurons of glia we’re interested in? And two, once we have that model and we understand the pathology, are we modeling some pathology that this patient has versus let’s say, a healthy control model? And then use therapeutics in this, in these cultures to see if we can have therapeutic benefits. So, you know, this is of course a pilot project, but that’s really, if successful, this is where we could take this, this, this, let’s say, modeling platform in microgravity condition.
Host: Is it, am I interpreting right that when you’re, when you’re talking about the, the models here in microgravity, you’re, you’re thinking that the way that you can do it is almost personalized testing? Meaning, you…
Shane Hagerty: Correct?
Host:…you can induce…that’s incredible. So you can, I mean, you can, you can test a, a complicated organoid model in microgravity that is not exactly, but very well represents a particular patient.
Shane Hagerty: That’s, that’s, that’s the, the goal of this.
Host: Wow.
Shane Hagerty: Like in our first, our first goal here, we are working with human neurons and glia, they’re not from a particular patient. It’s just proof of concept that when we take mature human neurons, and again, this is another thing we need to touch on with models in general, you know, back before we had induced pluripotent stem cells, when we did cell culture, we were growing embryonic neurons. We were growing embryonic astrocyte. These are not the cell types that are in the adult human pathology. They’re, you know, just because of maturity alone. And that can be misleading. I ran into that myself when I did a lot of work on growth factors, which are regulating, you know, human development, but may, may not have the same functions or the ability to function in the same way in the adult brain. So having a mature model, it’s important if you’re interested in adult neurological disorders. And, you know, we’ve been able to achieve that with induced pluripotent stem cells with longer differentiation protocols, better differentiation protocols. We can drive these neurons to become more and more mature, which is a good thing. And so, the idea here is we’re all, we’re taking the pre-differentiated mature human neurons and astrocyte, and we’re going to co-culture them in microgravity conditions based on other reports in, from microgravity and research on the ISS NL. They may self-assemble into a 3D assembloid. And that’s, you know, what we want to see. And as soon as we see that we can add this in the same experiment we’re going to add our precision gene therapy that should target the neurons and not the astrocyte, so we’ll get an answer about that as well. But if successful, the future is to take cell types from particular patients, I mean, you know, take a induced pluripotent stem cell from a patient, but make the cell types relevant for their pathology and then develop that model and test therapeutics. That could be where this leads to, depending on, as I said, this is obviously a pilot experiment.
Host: Right.
Shane Hagerty: But you can hear, I’m excited about seeing if it works or not.
Host: Yeah. Yeah. We’ll, we’ll, we’ll definitely get into that, right? That’s the whole thing is, this is, this is a trial. We’re, we’re trying, we’re trying to do it. I want to back up though and make sure that I understand, because I, I, I’m, I’m new to, to, to neuroscience and there are these…
Shane Hagerty: Sure.
Host:…I think when you’re talking about these models, you, you talked about these two distinct things and that, and, and one that you want to target and one that you don’t. And that’s…
Shane Hagerty: Yeah.
Host:…neurons and glia. In the model…
Shane Hagerty: Correct.
Host:…what are those different things and why do you want to target the neurons?
Shane Hagerty: Well, neurons are the cells responsible for, you know, centering our environment, executing, you know, motor functions. They’re processing information and they’re executing commands. So they’re firing these electrical signals in a process known as neuro-transmission. They’re all circuited together in complicated ways. So they’re the kind of executors of the central nervous system, but they can function without the astrocytes. The astrocytes are there to support the neurons, make sure they’re healthy. The astrocytes are important for having this blood-brain barrier to protect the brain from what’s circulating in our bodies, which ends up being a barrier for delivering drugs. But it’s, it’s important for other things. So they’re very different cell types. There’s also microglia. These are cell types that are the immune cells of the brain. So their job is to make sure that the, you know, detect any pathological, you know, proteins or pathogens and try to protect the brain. But sometimes they can, you know, because of a local inflammation or, or disease, they, they can actually have a negative impact. So these are all different functioning cell types that, that have particular roles. There’s oligodendrocytes, which are cell types that they wrapped in neurons in a seat, almost like an insulation of a, of a wire. And that increases the speed at which a neuron can send its signal to another cell. So they’re also essential for healthy brain function. So you can tell there’s a lot of different cell types. The neurons themselves have many different subtypes depending on where they’re located, their size, their shape. And there’s been, you know, a lot of neuroscience, you know, research over the last a hundred years, it’s been trying to characterize these different cell types and what they do and where they’re located and where they send their connections to and what connections they receive. So, you know, my, the point of being of targeting the neurons and not the astrocytes is, you know, if we think about the genome, you know, the many different genes, but they’re not all active in the, in, in, in the same cell type. But then there are some conserve pathways for one cell type and another cell type. And sometimes you want to tweak the function of a pathway in one cell, but not the other because it has a different role in different cell type. So if you only want to treat a particular cell type and not the rest of the body, because, you know, it’d be, there would be a therapeutic benefit to increasing the function of this pathway in the neuron. But there might be a problem if you do it in another cell type. That’s, you know, why we see things like side effects to drugs on America and things like that.
Host: Yeah.
Shane Hagerty: So if you want to be more precise in your therapy, because you know that that cell type will benefit from this treatment, you do want to risk treating other cell types, because they’re very different than their behavior. Like, for example, neurons are differentiated cells. They’re, once they become the cell type they are, they don’t, you know, continue to divide and things like that. They’re very fixed. That’s why it’s such a problem when they get damaged because you, they don’t, they don’t have the ability to, you know, on their own anyway, replace their last connections or, or regrow. So, but astrocytes are different. They actually can divide, they can replicate, they can proliferate, so they behave differently. So the, the signals that would make a neuron regrow might cause astrocytes to grow as well. And that might be a problem. So we, we try to, in different scenarios, deliver a therapeutic to the cell types that need it rather than other, and that’s kind of where the precision comes in. And it comes in, in two ways. You know, in the first way we, we spoke about, you can take a patient’s own cells and model their pathology by making a model, you know, a human assembloid model of their cell types and figure out why do their neurons have a certain pathology in, in these cultures. And the other type of precision, what we mean by that word is, we would precisely target a particular cell type or particular pathway in a, in a particular cell type. So there’s kind of two parts to this idea of precision neuroscience and this particular project.
Host: Yeah. It’s huge, right? That’s, and I think, I think having a better understanding of that really helps us to understand what precision means and why it’s so important and why complex models help us to have confidence in that level of precision.
Shane Hagerty: Correct.
Host: Now, I think the other thing you talked about that I wanted to circle back on was, we addressed this in the very beginning of our chat here, when it comes to AXONIS and, and what you guys are trying to do. But, we, we, we addressed that speed was one of those, one of those big, big items for you in developing things. And you, and when you talked about microgravity, one of the things you were talking about was this idea of self, self-assembling. The idea of microgravity helps you; your hypothesizing helps you with that speed. Can you help, can you help us characterize exactly what that means when you talked about rapid self-assembly and, and when you’re comparing these timelines? What, what is a, what is a ground process? When you talked about the lengthy process of, of, of developing a model. What, what does that timeline look like? And then, what is your hypothesis for how quickly a model can self-assemble, an assembloid can, can, can put itself together in orbit and, and sort of compare those timelines?
Shane Hagerty: You know, it’s, it’s a, it’s a great question. And you know, I, I alluded to it a little bit earlier. So I would say, one of the best models for studying human neurological disorders are organoids from that patient. So, as I said, you, you take a patient induced pluripotent stem cell, you make an organoid, you study their, the potential pathological processes of that patient’s neurological disorder. But these organoids can take many months to grow, because it takes a lot of time in culture to get to that level of differentiation. And they, you know, these are great models. I’m not denying that. And I think they’re a huge asset to the, to neuroscience research community and drug developers. But the idea of not waiting for the cell types to grow into these organoids, but to take the cell types that you’ve, you’ve pre-differentiated them. So, you know, there’s obviously a preparation part to do on Earth before you would, you know, do the, the 3D self-assembly part onward. But you take the different cell types of interest, they’re already differentiated, they’re already mature. You have the combination of cell types that make sense for what you’re trying to study. And then you, in microgravity conditions, and again, this hasn’t been tested for this particular cell types, but other cell types in microgravity come together to form these 3D structures. And that’s what we want to look at. And that, you know, happens much quicker and much shorter time scale than, as I said, if you wanted to grow an organoid from, from, from scratch.
Host: Are we talking about days, weeks, maybe one month? What’s the, what, what’s the…
Shane Hagerty: Exactly. So we, we kind of had to, and this was a process of refinement over the course of our preparation experiments to, you know, leading up to what we call an EVT (Endovascular Treatment) before we go to the ISS NL project. We want to streamline all our processes; we want to make it easier for the astronaut scientists to be able to conduct the experiments. So we had started, started out with a much longer timeline, but many factors fed into what we ended up with. One was the health of the cells over time. How do we make the protocol as easy as possible because another thing is, if it works, the easier the protocol is, the quicker, the easier it’s going to be to scale it, to do other things, right? So we wanted to come up with the simplest possible protocol where we don’t disturb the cells too much either during the process of the experiment. So based on what we read about the, what can happen in microgravity, and based on our preliminary experiments on the ground, obviously without being able to recapitulate the microgravity conditions, but looking at how the cells behave in a dish, how they behave when we add our therapeutic to the cultures, how long it takes to see the effect of our therapeutic in one cell type versus the other? We devise an experiment of only a couple of days for the, for the ISS NL and that’s for really efficiency. And, you know, it may be the case, it was naive, we should have left them for months and see what happened. But we did want to design the simplest, most efficient experiment to answer our questions based on what we spent a lot of time in our own lab optimizing for on-orbit operations. But I think it’ll be a huge benefit that we made it simple, right? Because if we want to do it again, if we want to take, you know, make this a screening platform for drug discovery, then the simpler the experimental processes, the more we can plug in different things to make it a little bit more complicated as we go. More cell types, more therapeutics, more, you know, more cultures grow, being grown in parallel. How do we scale it? And if the initial protocol is very complicated and you know, it takes many weeks or months, then, you know, we’re not necessarily making much of a benefit or an improvement on what we can already do on Earth. So the idea that it would be rapid, is, is, is, you know, for me that has to be rapid or we’re not going to maybe improve upon what we can already do here on, on the Earth.
Host: Sure. Yeah. Yeah. And that’s, that’s a really important distinction. And, and it’s, it’s, it’s significant. And I know you guys are, are paving the way, right? When it comes to this sort of neurological disorders and drug testing for this type of model. But, but you know, that, that level of speed and, and is, is, is, is pretty important. And I know you guys are making it simple, but it’ll be interesting to see how this thing evolves. When you talk about your experiment design, right, you said you’re, you try to make it simple and everything. Let’s, let’s go into that a little bit. Let’s go into what, you know, when, when you’re talking about what exactly is, is this experiment that’s going to be taking place, what does it look like? What, what are the containers? What’s the hardware? And are the astronauts going to interact with it? What’s the actual experiment on board station look like?
Shane Hagerty: The story behind our proposal and then, actually making it a realistic experiment was actually, that took about a year to go from what we thought was a good idea to what is physically possible on the space station. You know, maybe we should, we should have touched on that a little bit.
Host: Yeah, let’s do It.
Shane Hagerty: The reason we have the opportunity to do this is because AXONIS Therapeutics was part of a, an accelerator program known as MassChallenge. And every year MassChallenge has a, an award where they encourage their companies to propose a scientific experiment to be conducted on the ISS NL. And at the time, you know, we are obviously very much focused on the discoveries we’ve made in Boston Children’s Hospital Heart Medical School, how we’re going to make therapeutics for those? And, but this really encouraged us to think outside the box, right? You would, you know, it, it was a very, it was almost, it was too good of an opportunity to turn down in terms of there was funding designated to do this work. And initially we, we, we just talked to ourselves, “oh, we’re not a company that, you know, would work, you know, in space. So, you know, this isn’t for us.” But, you know, very quickly we thought about how do we actually make use of these different conditions to do something interesting, to do something we can’t do here? And that’s where the idea came from. And at that point, we hadn’t thought about how to make it, you know, operational on-orbit. But we had a plan of, as I just said, take the mature neurons and glia, make use of this 3D self-assembly that’s been happening in microgravity for other cell types, and see if we can get this 3D mature human brain assembloid model to, you know, be useful for studying therapeutics. And at the same time, test one of our therapeutics in the same experiments. But once we, you know, were successful in, in getting this grant award, then we had to really think about what would you actually use experimentally? What do the astronauts have access to? And you know, one, one thing we’re quite proud of is, before our project, there wasn’t the centrifuge on the ISS NL. Now there is, there’s a micro centrifuge that’s going to be shipped to the ISS NL as part of our project, because that was just something we have to have to make the experiment work.
Host: Cool.
Shane Hagerty: So there, you know, these are things you take for granted, obviously in your lab, you can’t take anything for granted up there. Everything, you know, we’re thinking about how, how everything is stored, how, how tight are the, the lids on different things, the volumes, every, and like, we have to work in a new culture container that you would never use, obviously on the Earth, these highly high-pressurized bio cells. We didn’t invent those. They were, they were something that were, we, we worked closely, but a number of different organizations and, you know, planning this, this project and, you know, basically bio server or partners and they suggested that if you want to run this cell culture experiment, you should use these bio cell devices. So they, that was a, you know, if, if they didn’t exist, we probably would have trouble making this experiment in reality. But they did exist. Then we have to adapt our culture protocols to grow ourselves in these bio cells. That took a lot of time. And, you know, and they’re quite difficult to work with, so we couldn’t do as much the cell culture as you’d like, you would possibly do on the ground. So then, we were trying to reduce the complexity of the steps, you know, how do we streamline everything? How do we optimize, how do we shorten the protocols, you know, and what, what, what’s the quickest timeline to getting the answer we’re looking for? So that was, that was a process, as I said, start out with a big idea. Let’s see if we can get this grant funding. We’re excited about it. It was just, you know, we, we, and then led into what we have today, which is, you know, a successful project today in terms of, you know, we, we proved through our EVT, which is a kind of a on ground final experiment. We do everything exactly like you’d expect the astronaut to do. That worked beautifully on Earth. But again, we did it, you know, with gravity conditions. We were using, you know, the, the conditions that the cells are normally happy with. But on, on the ISS NL, this is where hopefully, we’ll see the, what, what the microgravity will allow, which is the 3D central assembly, which we couldn’t do obviously in our lab. So that’s the part that will be, you know, the hypothesis to be tested. So I, you know, I hope that answered your question.
Host: A little bit. Yeah, yeah. I think I, I was thinking about, you know, is how it runs too, expanding on just the design just in general, you know? It sounds like…
Shane Hagerty: Yeah.
Host:…the way that you’re designing the hardware, I, do you need some sort of level of imagery or telemetry that gets, that gets fed to your lab…
Shane Hagerty: Correct.
Host:…so you understand what’s happening real-time, or are, is it just as simple as freezing the samples and shipping them back at some point in the future? So you can actually take a look in your lab and all you’re doing is just, you know, you’re working with the microgravity conditions and just kind of freezing it to look at later. What does that process look like?
Shane Hagerty: OK, let me, let, let’s revisit that then, in terms of step-wise process. And, you know, the, the reason we got to an experiment that, you know, we’ve increased the likelihood of a success on orbit is because, you know, weekly meetings with people who run these types of experiments before. And they really helped us to refine our experimental design. So here’s what we have to do. You know, we’re, we’re sending the cells frozen, and they’re, they’re, you know, these cells are happy in liquid nitrogen. And for a period of minus 80, before they’ll be grown in culture, and we’ve tested all those durations, how long will the cell tolerate this temperature? How long will it tolerate that temperature? What if the, the launch is delayed? What if it takes a bit more time for the astronauts to do the experiment versus this? Every single thing you would never think about in your, you would just do things like in the ideal protocol on Earth, right? You wouldn’t be trying to prepare against delays. You know, we can’t store it here for at this period because we don’t have a, a liquid nitrogen, you know, storage unit here. You know, so you are kind of changing, you’re almost changing protocols because you’re meeting the needs of the, getting the payloads to the ISS NL. So we were, you know, a lot of those things weren’t the most exciting experiments…
Host: Sure.
Shane Hagerty:…we had to do to make sure that our cargo, which are the neuron, which are the glia, these are already the pre-differentiated mature neurons and glia.
Host: Yeah.
Shane Hagerty: That was the process in itself. That was the standard project. We have to figure out how mature can we make them, that they will survive the freeze/thaw process? We, that was a very defined experiment. We did multiple different time points. It actually turned out they were too mature. They would have a trouble with that freeze/thaw. So when we brought, when they would be grown again on orbit, they wouldn’t be as healthy as we would like. So that was the whole process in itself. Then, we’re also sending our therapeutic gene therapy as an AAV gene therapy that needs to be, you know, have its own storage considerations. And, you know, then we’re thinking about the way that you load this bio cell is very different to how you’d ever work with a cell culture using these long needles, things like that. So the volumes is everything have to be adapted to this new system. The speed at which you can do things, the, as you said, we have to kind of, we have to request that this microcentrifuge go to the ISS NL. I think it would help the, that space station in future be able to do more of these types of cell culture experiments. Because for us, when the cart was frozen, right, it’s frozen in the media that protects the cells from that freeze/thaw process. But when the cells are like, they’re not very happy in that media. So we need to spin them out of that freezing media and put them into their growth media, which supports their viability and, and their, their state. So, that, we couldn’t get around not having a microcentrifuge for that step. So luckily that was, that was accommodated for the project. Then at the end of the project, there is a — there’s a lot of, for instance, microscopy to be done. That’s how we’re going to see if this worked or not. We’re going to do that in the live cells. That’s, that’s going to be part of the astronauts experiment.
Host: I see.
Shane Hagerty: We have the opportunity to actually video call into the ISS NL to be patterned that, so the, we’ve sent them a lot of images of what we hope that they will see, you know, this is what we, you’ll be looking for down the microscope. This doesn’t look like this. It might look like that. Here’s how best to look for, look for these assembloids in the, in the, in the culture, culture flask. And then, we also, because of our, our gene therapy as a fluorescent marker to show which cells it’s expressing in and not the other cells we’re using a green fluorescent protein. So the cells that got the therapeutic will be fluorescent green and the cells that don’t have it, which would hopefully be the astrocyte, we’ve already proven that on Earth. But, you know, again, this is another model. The model system on, on orbit. We will pick that up by a microscopy. We can also use a phase contrast microscopy, where we just look at the kind of, you know, the cells using the interplay of light. And we can get a sense of the structure of the assembloids. So they’re the types of images that are going to be taken during the experiment on orbit. At that point, the bio cell will be fixed, meaning the cells will be almost frozen in time. So you, you fixed them. So they kind of, that’s like a snapshot at that moment in time. You, you know, it, it does, you know, the cells are being killed, right? But they’re being fixed so that they don’t degrade. That, that fixed bio cell is going to be sent back to our lab where we’re going then going to take the assembloids out of the bio cell and do further microscopy. We’re going to be able to, you know, in the live, you can’t, you know, you can’t stain the live cells. You can, you can put one of these fluorescence proteins like GFP (Green Fluorescent Protein) into the live cell. They make the fluorescent protein. You can track it in, in, in the living cell, but you can’t add what are known as stains to look at one cell type versus the other. Look at certain, you know, our therapeutic is working on certain pathways. We, we’re going to look at markers for that. So there’ll be, once we get the cargo back from the ISS NL, we’re going to take out the, you know, the human model assembloid and do further stainings and histology to, you know, study what, what, what happened on, on, on the, on the ISS NL project.
Host: That’s awesome. I, I hope, I mean, I’m absolutely fascinated by this process. This, like, when you get down to the logistics of it, and I just, you just sort of lay out how complicated this process is from all of the testing ahead of time to make sure that this thing is ready for launch, it’s going to survive in microgravity. We kind of have a good idea of what we’re going to do. You have help along the way, like as you, as you were saying, people who have done science experiments on board. But still, you know, I think, how I wanted to sort of lead this to was an idea of just, just high-level, just microgravity research, right? I think, what’s interesting is you’re entering this world like many other researchers before you of, of microgravity — microgravity research and the complexities of, of what it takes to get things on orbit and the challenges that come with it, right? You have to talk about mass, you have to talk about size. You have to talk about these, these challenging delays. You have to do all of this remotely, right? You can’t just walk into the lab, right, because it’s, it’s orbiting. So there’s, there’s a lot of these challenges. And, and I’m curious to hear your perspective as a researcher doing research on board the International Space Station. Why? Right? So what I, what I’m, what I’m thinking about is, is, is, you thought about this idea ahead of time and you expected microgravity to have these, these promising to, to be promising in terms of what the microgravity environment can offer. You can only do it in orbit, right? It’s that, you can’t, you can’t generate microgravity on Earth. You have to do this on orbit. So I wonder, going through this process now, right? We’re, we’re ahead at the time we’re recording this, we’re ahead of NG-19 launch, where it’s actually going to be sent to the station, but understanding what it takes to do research and microgravity but comparing that to what it may promise and the future that that holds…
Shane Hagerty: Yeah.
Host:…I wonder how, I wonder how you view the value of microgravity research as a researcher yourself? Going through this process freshly, knowing the challenges, knowing the, the results, what are your views about microgravity research?
Shane Hagerty: Well, the reality is, is it’s not a, you know, it’s, it’s paradigm shifting in a way because when you’re, you know, conducting a neuroscience research, you don’t necessarily ask yourself the question of, how would this experiment behave? Or how would this model, you know, maybe be improved? Or what would be different if we tried this in microgravity conditions? It’s just not something that crosses your mind.
Host: Yeah.
Shane Hagerty: The, when we’re in MassChallenge, when we’re given the opportunity to apply for this funding award, the technology and space award, we were very proud to receive that. It forced us to sit down and think about things. And we had a lot of bad ideas before we narrowed down on what we ended up proposing here, we’re talking about today; this became much more feasible. Obviously, took a bit of research. What are people able to do? You know, a lot of people work on biomaterials or crystallization and things like that. But we, we need to think it a little bit more about what is biologically possible and what do people normally leverage microgravity for in terms of even animals or cells? And, you know, this, this 3D self-assembly of, of cells was the, the most exciting aspect. And as I said, we’ve been limited in treating neurological disorders because it’s been difficult to study them. It’s been difficult to model them. You can’t model the pathology. How do you expect to develop, understand it first, but then develop therapeutics to try to, you know, address the pathology that you’re, you, you’re basically studying? So, and you know, as I said, the precision part comes from the fact that we can take the, the iPSC (induced pluripotent stem cells) from any patient and try to model their pathology. So that, that’s the, the next level of that. But the, as I said, it just hadn’t crossed my mind. You know, maybe other people will do that. You know, I’d love to take a survey and does anybody on every now and again decide when they’re working in their space, what would this be like in microgravity conditions? I, I would almost, it should be like, we have to have some sort of campaign just to force everybody to sit down for an hour and ask themselves that question. Whatever field they’re in, whatever model they’re working on. If you were to run this in microgravity, you know, what could, what could be improved, because that’s what it takes sometimes, right? Like the, the, the progress of induced pluripotent stem cells. I mentioned the differentiation protocols. Now, there’s directing differentiation with the, you know, genetic pre-programming organized, amazing progress. The field is, you know, that’s, that’s huge for the field. But again, it at a certain point, you know, it gets to a point where, OK, where’s the next kind of, you know, step on this? How can we push it to another level? And, you know, always limited by tools and technology, but now we’ve added in this extra, you know, variable or, or something we can leverage within the microgravity conditions to see if we can improve upon this technology in the ways I mentioned, right? Can we rapidly make them become 3D? Can we take the very mature cells from the very start and all the different cell types we’re interested in mixed them together, have them assembled in the 3D assembloid model of the human brain? And once we do that, how do they behave? Will they be, will there be clear pathologies in the patient’s model versus the maybe healthy control? If we see something like that, can we do drug screening on those phenotypes? So that’s kind of the exciting part. You know, I’m obviously getting carried away. We haven’t seen if it works to the level, I hope it will, yet. But, you know, we’ve taken every measure possible over the last year or so to de-risk the experiment, because we only get one shot at it, right?
Host: Right?
Shane Hagerty: So we, that’s why we’ve been, you know, painstakingly testing every part of it all, because we don’t want, you know, to, to run into any problems when, when the astronauts go to run the protocol. And it’s a very defined protocol, very step-wise. Every part of it, you know, nothing’s taken for granted. We can’t get up there and do it ourselves. So we just need to make it as clear as possible what we’re trying to do, what we’re looking for. You know, I’m glad that there’s an ability to be part of the imaging process at the end, so we can guide at that part. You know, maybe I should’ve tried to convince them to let me go up there as well. I’d love to go up there myself. But the, the, that’s, that’s, you know, as I said, it’s, it could be paradigm shifting or, you know, maybe just, you know, we’ll have to see how it turns out. But I’m very excited about it. I see all the time about people wanting to build infrastructure in space. You know, it’s becoming a new horizon for manufacturing. So why not, if this works, right? If it, if it works nicely, it’s a, it’s an efficient process. There’s obviously some preparatory steps you need to do on the ground in terms of getting the different cell types you’re interested prepared, but then why not have the screening platform on orbit, if it allows us to do something we can’t do here on Earth?
Host: Yeah. I, I, you’re very measured in your response, but what I’m, what I’m gathering is we, you know, it’s, it’s almost like we got to try, right? If you want to make that progress.
Shane Hagerty: Exactly.
Host: If we got to make, if we’re going to make the progress we have and this, this has the potential to offer at least a step in the progress, then, then, then let’s try it. And so, I think it’s, I, I think it’s a worthwhile endeavor. It’s, it’s so complicated. But, but I think, for me, at least from what I’m gathering for you, there, there is some significant promise to this, that, that is worth, that is worth trying to do it in microgravity. It could, it could lead to, it could lead to better models and therefore, better, you know, drug testing, faster drug testing. All that sort of helps those with neurological disorders. And I think that, that, you know, to me, it’s, it seems worth it.
Shane Hagerty: 100%. You know, this, this is obviously grant-funded pilot study…
Host: Sure.
Shane Hagerty:…but it’ll be a pivotal proof of concept, right? So if we can prove that we can, you know, do this — maybe, you know, it’s, it’s a simplified version of, you know, what I imagine would be very powerful. But we need that proof of concept to convince people that it’s worth trying again, it may be worth scaling it up, you know, put more minds together to see if there’s any other improvements that can be made. You know, this, these are, this is why we, you know, it’s an exploratory research project, obviously has a lot of applications. So we’re excited to see how it turns out.
Host: Yeah, absolutely. And I think, you know, like, like, you said, it was, it was you, it was many, many others that worked very, very hard…
Shane Hagerty: Correct.
Host:…to get, to get ready for, to get this experiment ready. To, to see it through. And so, I’d just like to say by, you know, Shane, by just thanking you for your time, but then also, you know, just congratulations to you and your team to, to getting it this far at this time that we’re recording this. We’re ahead of launch. So I’m wishing you guys the best with launch and with actually integrating the experiment with the astronauts and testing it out onboard the International Space Station. Very exciting times. So I appreciate you coming on the podcast today to help us to understand what this is and, and what it takes to do research in microgravity and it’s, it’s super interesting stuff. So appreciate your time, Shane. Thank you.
Shane Hagerty: I appreciate that. And do you mind me just, just before I jump off, I need to, you know, acknowledge everybody who put a lot of effort…
Host: Please. Of course.
Shane Hagerty:…into this project, you know, the, my co-investigators, Joanna Stanicka, Lisa McKerracher, who put the proposal together in the first place. There was a very talented scientist in the lab, Tia Dey who, you know, with me, had to try to test out all these different things that you wouldn’t normally do for, you know, your routine experiments. But she maintained her enthusiasm and curiosity about, about where this could go. We also, I don’t know if you, if it will ever appear on, on this podcast or where it’ll ever become public, but we have another team member, Eilah who prepared a really nice mission badge of, of what we’re doing…
Host: Oh, very cool.
Shane Hagerty:…which we’re very, we’re very proud of. Apparently, that may be stick, stuck on the cargo on its way up to the ISS NL. So all, all the different parts have been important for, you know, executing on, on the, on the grant proposal, and we’re excited to see the results and I appreciate your time today. And I meant to say that, you know, must be one of the coolest names for a podcast I’ve ever come across, you know, it’s a great name. And another, another side point, you know, I’m from Ireland and, you know, it’s, it’s literally like science fiction to even be in, in a, in this kind of situation where an experiment we’ve devised as a team, you know, will, will be, will be going up to the ISS NL. So it’s certainly beyond my dreams and it’s, it’s great to see that there’s an infrastructure and an appetite to push the boundaries of science in this way…
Host: Absolutely. Absolutely.
Shane Hagerty:…in the U.S.
Host: Yeah. Yeah. And I’m, I’m so happy that you and your team are a part of it. So thanks again, Shane, really appreciate the time.
Shane Hagerty: Thank you.
[Music]
Host: Hey, thanks for sticking around. Really interesting conversation with Shane today. He did such a good job. This is such a complicated area to navigate neurological diseases and, and modeling, but I think he did a really good job of breaking it down and helping me to, to understand exactly what’s going on here. And it was absolutely fascinating. So I hope you were just as fascinated as I am. We have conversations like this a lot; experiments on board the International Space Station, and you can check out our full collection on NASA.gov/podcasts. In fact, if you go to the website, we actually put together a collection of just episodes on the International Space Station where there are a lot of experiments, and you can listen to any one of those in no particular order. Just to understand some of the research that’s happening in low-Earth orbit. If you want to talk to us though, or ask us a question, make sure it, may even make a suggestion for an episode that you think would be really interesting to cover on Houston We Have a Podcast, we’re on social media on the NASA Johnson Space Center pages of Facebook, Twitter, and Instagram. You can use the hashtag #AskNASA to suggest an episode or ask a question. But if you want to direct it towards us, just make sure you mention us in that post, Houston We Have a Podcast. This episode was recorded on April 17th, 2023. Thanks to Will Flato, Pat Ryan, Heidi Lavelle, Belinda Pulido, and Jaden Jennings and Destiny Doran. And of course, thanks again to Shane Hegarty for taking the time to come on the show. Give us a rating and feedback on whatever platform you’re listening to us on and tell us what you think of our podcast. We’ll be back next week.