Sylvain Costes
Project Manager, Principal Investigator
Phone: (650) 604-5343
Email: Sylvain.V.Costes@nasa.gov
Affiliation: Space Biosciences Research Branch
Professional Background
Biography
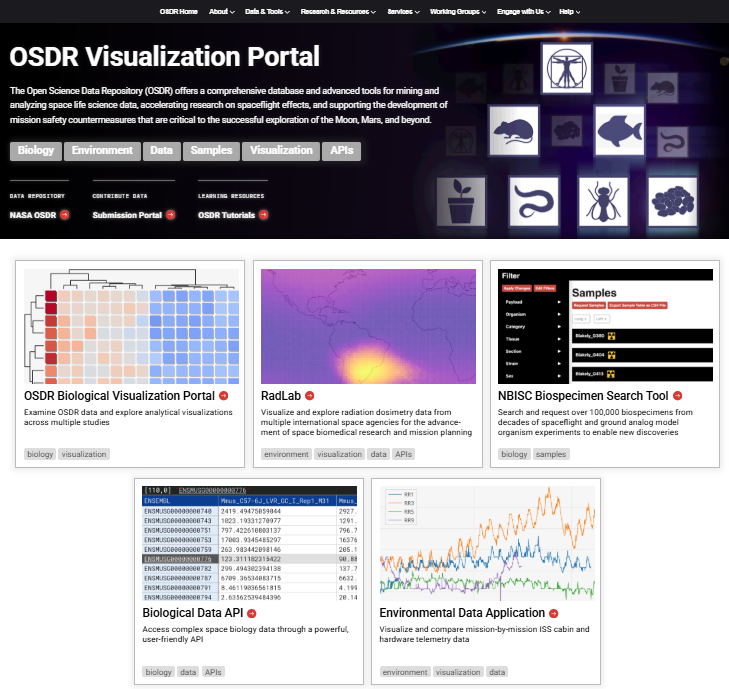
Dr. Costes is a senior research scientist leading the Ames radiation biophysics laboratory. He obtained his Ph.D. in the Nuclear Engineering Department at the University of California, Berkeley, where he studied radiation biology in 1999. Dr. Costes has spent his career leading multidisciplinary research teams in both academic and government scientific institutions. As a bioimaging specialist and microscopist, he developed at the National Cancer Institue (NCI) gold standard spatial statistics algorithms to quantify protein-protein interactions (I.e. colocalization). As a staff scientist at the Lawrence Berkeley National Lab (LBNL), he was modeling cancer risk for the NASA Human research program and developing biomarkers for the DOE low dose program. As the CEO and co-founder of Exogen Biotechnology Inc., a spin-off startup from LBNL, he played a critical role in the success of the company, providing leadership, vision, and scientific direction. Exogen sought to revolutionize the field of personal diagnostics using DNA integrity as its main biomarker. His key responsibility was to raise capital for the company and interact with the FDA (Food and Drug Administration) to establish products and services in compliance with all regulatory requirements. He is now the project manager for Open Science at NASA Biological and Physical Sciences Division (BPS), where he leads the systems biology research, AI/ML modeling initiative and the software development for two large NASA data systems: the GeneLab Omics repository and the ALSDA repository for physiological data from spaceflight relevant experiments. Dr. Costes is also the Point of Contact for BPS at the NASA Science Mission Directorate, working with the Open Source Science Initiative Council and the SMD Artificial Intelligence (AI) Initiative working group. Dr. Costes is one of the NASA POC for the Data & Innovation Task Force led by the Office of Science and Technology Policy at the White House, where he pushes forward the work done at NASA for the Cancer Moonshot.
Awards and Activities
- 2023: Member of the Cancer Cabinet | Data & Innovation Task Force – Office of Science and Technology Policy | The White House
- 2023: NASA Human Research Program Significant Contributor Award
- “For advancing open science to include massive data and sample sets from the HRO-funded model organism studies in ALSDA and NBISC repositories and making them publicly accessible via a novel unified portal”
- 2021: NASA Exceptional Scientific Achievement Medal
- “For exceptional discoveries that enhance our understanding of the effects of long-term spaceflight on biological systems and human health through GeneLab global collaboration.”
- 2021: NASA Team Award: GeneLab
- 2020: NASA Ames Team Award: GeneLab
- 2018: NASA Exceptional Achievement Medal
- “For transforming GeneLab into an efficient, impactful, and versatile repository for use by the biological research community.”
- 2016: Berkeley Lab – Lead strategy in Biosciences for Health Pillar: Impact of environmental challenges on human biology.
- 2015-2016: Berkeley Lab – Leadership team for the Institute for Resilient Communities (http://www.irc-berkeley.org/)
- 2014: Berkeley Visionary Award – for entrepreneurship, Sept 2014
- 2013: Associate Editor for the journal of the Radiation Research Society, Sept 2013
- 2012: Berkeley Lab – Emerging Leader Program: Lawrence Berkeley National Laboratory / Haas School of Business Executive Training – UC Berkeley
- 2011: Elected Radiation Research Society Physics Councilor, 2011-2013
- 2007: Berkeley Lab – 2007-2008 Outstanding Achievement Award, Cancer System Biology Division
- University of California at Berkeley
- 1997-1998 Outstanding Graduate Student Instructor in Nuclear Physics & Biophysics University of California at Berkeley
- 1996-1997 Earl C. Anthony Fellowship and Regents Fellowship
Education
1994: M.S. Physics & Mathematics, PHELMA, Institut Polytechnique, Grenoble, France
1994: M.S. Nuclear Engineering, Texas A&M University, College Station, TX
1999: Ph.D. Nuclear Engineering, University of California, Berkeley, CA
2000: Postdoctoral Fellow, Dept of Mathematics, UC Berkeley, CA
Lead for the Radiation Biophysics Lab uses computational and experimental methods to understand how ionizing radiation impacts health at the level ranging from single molecules to whole organisms. We study the impacts of deep space radiation and combined exposures to other spaceflight stressors on the immune system and the neurovascular system, with advanced lab on a chip technology and various sources of ionizing radiation. We also work on identifying peripheral blood-based biomarkers of individual sensitivity to ionizing radiation in humans and model organisms, with a particular interest in genomic associations to radiation resilience. We are also a proud training lab for the next generation of scientists and actively focus on supporting postdoctoral scholars and research associates.
Current research interests include:
- Computational modeling of DNA damage and repair responses to ionizing radiation.
- Demographic and genomic associations of individual sensitivity to ionizing radiation in mouse and human populations, using skin and blood as surrogate tissues.
- Transcriptomic profiles associated with exposure to ionizing radiation.
- Differences between chronic and acute exposures to ionizing radiation.
- Circulating factors (exosomes, cytokines) as potential biomarkers of ionizing radiation exposure and individual sensitivity.
- Utilizing high-throughput human organ-on-a-chip models of the central nervous system and the blood-brain barrier to investigate the neurovascular outcomes of deep space radiation exposure.
Radiation Biophysics Lab Team Members
Principal Investigator / Research Scientist: Egle Cekanaviciute, Ph.D.
Research Associate: Estrella Passerat de la Chapelle (PhD Student)
Postdoctoral Fellow: Amber M. Paul, PhD (former)
Postdoctoral Fellow: Eloise Pariset, Ph.D. (former)
Scientist: Siddhita Mhatre: Ph.D. (former)
Scientist: Ivan G. Paulino Lima, Ph.D. (former)
Visiting Scientist: Janani Iyer, Ph.D. (former)
Research Associate: Sherina Malkani (former)
Research Associate: Alejandra Lopez-Macha (former)
Software Engineer: Vanesa Gomez Gonzalez (former)
Research Associate, Sonali Verma (former)
Staff Scientist, Connie Tsai Pasternak, Ph.D. (former)
Patents
- High throughput DNA damage quantification of human tissue with home-based collection device (2018)
SV Costes, J Tang, SM Yannone
US Patent 9,931,634 - Devices and methods for determining sensitivity to radiation
SV Costes, R Gomez-Sjoberg, SM Yannone
US Patent App. 14/378,617
Links to Professional Profiles
News media coverage
- http://newscenter.lbl.gov/2015/09/01/time-lapse-dna-damage/
- http://newscenter.lbl.gov/2014/02/06/berkeley-lab-startup-wants-to-know-how-damaged-your-dna-is/
- http://newscenter.lbl.gov/2011/12/20/low-dose-radiation/
Podcast
Videos
- 2019 AAAS NASA Press conference
- Genetic Data from Space | Genes in Space
- Visionary Award 2014
- Science at the Theater: 8 Big Ideas in Oakland, CA
- Science at the Theater: Next Big Tech Idea Revealed
- Google TechTalks
Publications
1. Wilson, L.J., et al., Machine intelligence for radiation science: summary of the Radiation Research Society 67th annual meeting symposium. Int J Radiat Biol, 2023. 99(8): p. 1291-1300.
2. Scott, R.T., et al., Biomonitoring and precision health in deep space supported by artificial intelligence. Nature Machine Intelligence, 2023. 5(3): p. 196-207.
3. Sanders, L.M., et al., Biological research and self-driving labs in deep space supported by artificial intelligence. Nature Machine Intelligence, 2023. 5(3): p. 208-219.
4. Sanders, L.M., et al., Batch effect correction methods for NASA GeneLab transcriptomic datasets. Frontiers in Astronomy and Space Sciences, 2023. 10.
5. Morris, J.H., et al., The scalable precision medicine open knowledge engine (SPOKE): a massive knowledge graph of biomedical information. Bioinformatics, 2023. 39(2).
6. Cekanaviciute, E., et al., Mouse genomic associations with in vitro sensitivity to simulated space radiation. Life Sci Space Res (Amst), 2023. 36: p. 47-58.
7. Verma, S.D., et al., Astrocytes regulate vascular endothelial responses to simulated deep space radiation in a human organ-on-a-chip model. Front Immunol, 2022. 13: p. 864923.
8. Overbey, E.G., et al., Challenges and considerations for single-cell and spatially resolved transcriptomics sample collection during spaceflight. Cell Rep Methods, 2022. 2(11): p. 100325.
9. Mhatre, S.D., et al., Artificial gravity partially protects space-induced neurological deficits in Drosophila melanogaster. Cell Rep, 2022. 40(10): p. 111279.
10. Vangay, P., et al., Microbiome Metadata Standards: Report of the National Microbiome Data Collaborative’s Workshop and Follow-On Activities. mSystems, 2021. 6(1).
11. Vangay, P., et al., Correction for Vangay et al., “Microbiome Metadata Standards: Report of the National Microbiome Data Collaborative’s Workshop and Follow-On Activities”. mSystems, 2021. 6(3).
12. Penninckx, S., et al., Quantification of radiation-induced DNA double strand break repair foci to evaluate and predict biological responses to ionizing radiation. NAR Cancer, 2021. 3(4).
13. Penninckx, S., et al., Considering Cell Proliferation to Optimize Detection of Radiation-Induced 53BP1 Positive Foci in 15 Mouse Strains Ex Vivo. Radiat Res, 2021. 195(1): p. 47-59.
14. Pariset, E., et al., Ionizing radiation-induced risks to the central nervous system and countermeasures in cellular and rodent models. Int J Radiat Biol, 2021. 97(sup1): p. S132-S150.
15. Overbey, E.G., et al., NASA GeneLab RNA-seq consensus pipeline: standardized processing of short-read RNA-seq data. iScience, 2021. 24(4): p. 102361.
16. Nguyen, H., et al., CPA: a web-based platform for consensus pathway analysis and interactive visualization. Nucleic Acids Res, 2021. 49(W1): p. W114-W124.
17. Nelson, C.A., et al., Knowledge Network Embedding of Transcriptomic Data from Spaceflown Mice Uncovers Signs and Symptoms Associated with Terrestrial Diseases. Life (Basel), 2021. 11(1).
18. Michalettou, T.D., et al., A Meta-Analysis of the Effects of High-LET Ionizing Radiations in Human Gene Expression. Life (Basel), 2021. 11(2).
19. McDonald, J.T., et al., The Great Deceiver: miR-2392’s Hidden Role in Driving SARS-CoV-2 Infection. bioRxiv, 2021.
20. McDonald, J.T., et al., Role of miR-2392 in driving SARS-CoV-2 infection. Cell Rep, 2021. 37(3): p. 109839.
21. Cahill, T., et al., Mammalian and Invertebrate Models as Complementary Tools for Gaining Mechanistic Insight on Muscle Responses to Spaceflight. Int J Mol Sci, 2021. 22(17).
22. Berrios, D.C., et al., NASA GeneLab: interfaces for the exploration of space omics data. Nucleic Acids Res, 2021. 49(D1): p. D1515-D1522.
23. Barker, R., et al., Rad-Bio-App: a discovery environment for biologists to explore spaceflight-related radiation exposures. NPJ Microgravity, 2021. 7(1): p. 15.
24. Afshinnekoo, E., et al., Fundamental Biological Features of Spaceflight: Advancing the Field to Enable Deep-Space Exploration. Cell, 2021. 184(24): p. 6002.
25. Willis, C.R.G., et al., Comparative Transcriptomics Identifies Neuronal and Metabolic Adaptations to Hypergravity and Microgravity in Caenorhabditis elegans. iScience, 2020. 23(12): p. 101734.
26. Scott, R.T., et al., Advancing the Integration of Biosciences Data Sharing to Further Enable Space Exploration. Cell Rep, 2020. 33(10): p. 108441.
27. Rutter, L., et al., A New Era for Space Life Science: International Standards for Space Omics Processing. Patterns (N Y), 2020. 1(9): p. 100148.
28. Pariset, E., et al., 53BP1 Repair Kinetics for Prediction of In Vivo Radiation Susceptibility in 15 Mouse Strains. Radiat Res, 2020. 194(5): p. 485-499.
29. Pariset, E., et al., DNA Damage Baseline Predicts Resilience to Space Radiation and Radiotherapy. Cell Rep, 2020. 33(10): p. 108434.
30. Nikitaki, Z., et al., In Situ Detection of Complex DNA Damage Using Microscopy: A Rough Road Ahead. Cancers (Basel), 2020. 12(11).
31. McDonald, J.T., et al., NASA GeneLab Platform Utilized for Biological Response to Space Radiation in Animal Models. Cancers (Basel), 2020. 12(2).
32. Malkani, S., et al., Circulating miRNA Spaceflight Signature Reveals Targets for Countermeasure Development. Cell Rep, 2020. 33(10): p. 108448.
33. Lai Polo, S.H., et al., RNAseq Analysis of Rodent Spaceflight Experiments Is Confounded by Sample Collection Techniques. iScience, 2020. 23(12): p. 101733.
34. da Silveira, W.A., et al., Comprehensive Multi-omics Analysis Reveals Mitochondrial Stress as a Central Biological Hub for Spaceflight Impact. Cell, 2020. 183(5): p. 1185-1201 e20.
35. Afshinnekoo, E., et al., Fundamental Biological Features of Spaceflight: Advancing the Field to Enable Deep-Space Exploration. Cell, 2020. 183(5): p. 1162-1184.
36. Ray, S., et al., GeneLab: Omics database for spaceflight experiments. Bioinformatics, 2019. 35(10): p. 1753-1759.
37. Penninckx, S., et al., Dose, LET and Strain Dependence of Radiation-Induced 53BP1 Foci in 15 Mouse Strains Ex Vivo Introducing Novel DNA Damage Metrics. Radiat Res, 2019. 192(1): p. 1-12.
38. Ochola, D.O., et al., Persistence of Gamma-H2AX Foci in Bronchial Cells Correlates with Susceptibility to Radiation Associated Lung Cancer in Mice. Radiat Res, 2019. 191(1): p. 67-75.
39. Beheshti, A., et al., Exploring the Effects of Spaceflight on Mouse Physiology using the Open Access NASA GeneLab Platform. J Vis Exp, 2019(143).
40. Beheshti, A., et al., GeneLab Database Analyses Suggest Long-Term Impact of Space Radiation on the Cardiovascular System by the Activation of FYN Through Reactive Oxygen Species. Int J Mol Sci, 2019. 20(3).
41. Beheshti, A., et al., Multi-omics analysis of multiple missions to space reveal a theme of lipid dysregulation in mouse liver. Sci Rep, 2019. 9(1): p. 19195.
42. Ray, S., et al., Comparing Photon and Charged Particle Therapy Using DNA Damage Biomarkers. Int J Part Ther, 2018. 5(1): p. 15-24.
43. McDonald, J.S., et al., Gadolinium-enhanced cardiac MR exams of human subjects are associated with significant increases in the DNA repair marker 53BP1, but not the damage marker gammaH2AX. PLoS One, 2018. 13(1): p. e0190890.
44. Cortese, F., et al., Vive la radioresistance!: converging research in radiobiology and biogerontology to enhance human radioresistance for deep space exploration and colonization. Oncotarget, 2018. 9(18): p. 14692-14722.
45. Cekanaviciute, E., S. Rosi, and S.V. Costes, Central Nervous System Responses to Simulated Galactic Cosmic Rays. Int J Mol Sci, 2018. 19(11).
46. Berrios, D.C., A. Beheshti, and S.V. Costes, FAIRness and Usability for Open-access Omics Data Systems. AMIA Annu Symp Proc, 2018. 2018: p. 232-241.
47. Beheshti, A., et al., A microRNA signature and TGF-beta1 response were identified as the key master regulators for spaceflight response. PLoS One, 2018. 13(7): p. e0199621.
48. Beheshti, A., et al., NASA GeneLab Project: Bridging Space Radiation Omics with Ground Studies. Radiat Res, 2018. 189(6): p. 553-559.
49. Beheshti, A., et al., Global transcriptomic analysis suggests carbon dioxide as an environmental stressor in spaceflight: A systems biology GeneLab case study. Sci Rep, 2018. 8(1): p. 4191.
50. Paul-Gilloteaux, P., et al., Optimizing radiotherapy protocols using computer automata to model tumour cell death as a function of oxygen diffusion processes. Sci Rep, 2017. 7(1): p. 2280.
51. Colmenares, S.U., et al., Drosophila Histone Demethylase KDM4A Has Enzymatic and Non-enzymatic Roles in Controlling Heterochromatin Integrity. Dev Cell, 2017. 42(2): p. 156-169 e5.
52. Swenson, J.M., et al., The composition and organization of Drosophila heterochromatin are heterogeneous and dynamic. Elife, 2016. 5.
53. Sridharan, D.M., et al., Evaluating biomarkers to model cancer risk post cosmic ray exposure. Life Sci Space Res (Amst), 2016. 9: p. 19-47.
54. Heuskin, A.C., et al., Simulating Space Radiation-Induced Breast Tumor Incidence Using Automata. Radiat Res, 2016. 186(1): p. 27-38.
55. Adams, C.J., et al., The Trp53 delta proline (Trp53DeltaP) mouse exhibits increased genome instability and susceptibility to radiation-induced, but not spontaneous, tumor development. Mol Carcinog, 2016. 55(9): p. 1387-96.
56. Tang, J., et al., Genetic Background Modulates lncRNA-Coordinated Tissue Response to Low Dose Ionizing Radiation. Int J Genomics, 2015. 2015: p. 461038.
57. Tang, j., et al., Mathematical Modeling for DNA Repair, Carcinogenesis and Cancer Detection, in Genomic Instability and Cancer Metastasis. 2015, Springer Science & Business Media. p. 75–93.
58. Sridharan, D.M., et al., Understanding cancer development processes after HZE-particle exposure: roles of ROS, DNA damage repair and inflammation. Radiat Res, 2015. 183(1): p. 1-26.
59. Georgescu, W., et al., Characterizing the DNA Damage Response by Cell Tracking Algorithms and Cell Features Classification Using High-Content Time-Lapse Analysis. PLoS One, 2015. 10(6): p. e0129438.
60. Vadhavkar, N., et al., Combinatorial DNA damage pairing model based on X-ray-induced foci predicts the dose and LET dependence of cell death in human breast cells. Radiat Res, 2014. 182(3): p. 273-81.
61. Tang, J., et al., Irradiation of juvenile, but not adult, mammary gland increases stem cell self-renewal and estrogen receptor negative tumors. Stem Cells, 2014. 32(3): p. 649-61.
62. Park, C.C., et al., Rapid and automated multidimensional fluorescence microscopy profiling of 3D human breast cultures. Integr Biol (Camb), 2013. 5(4): p. 681-91.
63. Chiolo, I., et al., Nuclear dynamics of radiation-induced foci in euchromatin and heterochromatin. Mutat Res, 2013. 750(1-2): p. 56-66.
64. Neumaier, T., et al., Evidence for formation of DNA repair centers and dose-response nonlinearity in human cells. Proc Natl Acad Sci U S A, 2012. 109(2): p. 443-8.
65. Nam, J., et al., Targeting Beta-1 Integrin Suppresses Invasive Recurrence in a 3-dimensional Model of Radiation Treated Ductal Carcinoma In situ. International Journal of Radiation Oncology*Biology*Physics, 2012. 84(3): p. S143.
66. Dunleavy, E.M., et al., The cell cycle timing of centromeric chromatin assembly in Drosophila meiosis is distinct from mitosis yet requires CAL1 and CENP-C. PLoS Biol, 2012. 10(12): p. e1001460.
67. Tang, J., et al., Phenotypic transition maps of 3D breast acini obtained by imaging-guided agent-based modeling. Integr Biol (Camb), 2011. 3(4): p. 408-21.
68. Spencer, V.A., et al., Depletion of nuclear actin is a key mediator of quiescence in epithelial cells. J Cell Sci, 2011. 124(Pt 1): p. 123-32.
69. Maxwell, C.A., et al., Interplay between BRCA1 and RHAMM regulates epithelial apicobasal polarization and may influence risk of breast cancer. PLoS Biol, 2011. 9(11): p. e1001199.
70. Groesser, T., et al., Persistence of gamma-H2AX and 53BP1 foci in proliferating and non-proliferating human mammary epithelial cells after exposure to gamma-rays or iron ions. Int J Radiat Biol, 2011. 87(7): p. 696-710.
71. Chiolo, I., et al., Double-strand breaks in heterochromatin move outside of a dynamic HP1a domain to complete recombinational repair. Cell, 2011. 144(5): p. 732-44.
72. Andarawewa, K.L., et al., Lack of radiation dose or quality dependence of epithelial-to-mesenchymal transition (EMT) mediated by transforming growth factor beta. Int J Radiat Oncol Biol Phys, 2011. 79(5): p. 1523-31.
73. Mukhopadhyay, R., et al., Promotion of variant human mammary epithelial cell outgrowth by ionizing radiation: an agent-based model supported by in vitro studies. Breast Cancer Res, 2010. 12(1): p. R11.
74. Ghajar, C.M., et al., Mesenchymal cells stimulate capillary morphogenesis via distinct proteolytic mechanisms. Exp Cell Res, 2010. 316(5): p. 813-25.
75. Costes, S.V., et al., Spatiotemporal characterization of ionizing radiation induced DNA damage foci and their relation to chromatin organization. Mutat Res, 2010. 704(1-3): p. 78-87.
76. Andarawewa, K.L., et al., Persistent Phenotypic Responses of Human Mammary Epithelial Cells Induced by Ionizing Radiation. Acta Medica Nagasakiensia, 2009. 53(Suppl. S): p. 61-63.
77. Ponomarev, A.L., S.V. Costes, and F.A. Cucinotta, Stochastic properties of radiation-induced DSB: DSB distributions in large scale chromatin loops, the HPRT gene and within the visible volumes of DNA repair foci. Int J Radiat Biol, 2008. 84(11): p. 916-29.
78. Maxwell, C.A., et al., Targeted and nontargeted effects of ionizing radiation that impact genomic instability. Cancer Res, 2008. 68(20): p. 8304-11.
79. Barkan, D., et al., Inhibition of metastatic outgrowth from single dormant tumor cells by targeting the cytoskeleton. Cancer Res, 2008. 68(15): p. 6241-50.
80. Costes, S.V., et al., Image-based modeling reveals dynamic redistribution of DNA damage into nuclear sub-domains. PLoS Comput Biol, 2007. 3(8): p. e155.
81. Andarawewa, K.L., et al., Ionizing radiation predisposes nonmalignant human mammary epithelial cells to undergo transforming growth factor beta induced epithelial to mesenchymal transition. Cancer Res, 2007. 67(18): p. 8662-70.
82. Fleisch, M.C., et al., Intensity-based signal separation algorithm for accurate quantification of clustered centrosomes in tissue sections. Microsc Res Tech, 2006. 69(12): p. 964-72.
83. Costes, S.V., et al., Imaging features that discriminate between foci induced by high- and low-LET radiation in human fibroblasts. Radiat Res, 2006. 165(5): p. 505-15.
84. Barcellos-Hoff, M.H. and S.V. Costes, A systems biology approach to multicellular and multi-generational radiation responses. Mutat Res, 2006. 597(1-2): p. 32-8.
85. Daelemans, D., et al., Kinetic and molecular analysis of nuclear export factor CRM1 association with its cargo in vivo. Mol Cell Biol, 2005. 25(2): p. 728-39.
86. Cho, E., S. Costes, and S. Lockett, Simple protocols for quantitative characterization of optical microscopy performance. Biophysical Journal, 2005. 88(1): p. 344A.
87. Muriaux, D., et al., Role of murine leukemia virus nucleocapsid protein in virus assembly. J Virol, 2004. 78(22): p. 12378-85.
88. Daelemans, D., et al., In vivo HIV-1 Rev multimerization in the nucleolus and cytoplasm identified by fluorescence resonance energy transfer. J Biol Chem, 2004. 279(48): p. 50167-75.
89. Costes, S.V., et al., Automatic and quantitative measurement of protein-protein colocalization in live cells. Biophys J, 2004. 86(6): p. 3993-4003.
90. Catalfamo, M., et al., Human CD8+ T cells store RANTES in a unique secretory compartment and release it rapidly after TcR stimulation. Immunity, 2004. 20(2): p. 219-30.
91. Yang, H.S., et al., The transformation suppressor Pdcd4 is a novel eukaryotic translation initiation factor 4A binding protein that inhibits translation. Molecular and Cellular Biology, 2003. 23(1): p. 26-37.
92. Ortiz De Solorzano, C., et al., Applications of quantitative digital image analysis to breast cancer research. Microsc Res Tech, 2002. 59(2): p. 119-27.
93. Costes, S. and M.H. Barcellos-Hoff, Radiation quality and tissue-specific microenvironments following exposure to 1 GeV/amu Fe. Adv Space Res, 2002. 30(4): p. 865-70.
94. Costes, S., et al., Large-Mutation Spectra Induced at Hemizygous Loci by Low-LET Radiation: Evidence for Intrachromosomal Proximity Effects. Radiation Research, 2001. 156(5): p. 545-557.
95. Costes, S., C.H. Streuli, and M.H. Barcellos-Hoff, Quantitative image analysis of laminin immunoreactivity in skin basement membrane irradiated with 1 GeV/nucleon iron particles. Radiat Res, 2000. 154(4): p. 389-97.
96. Bolch, W.E., et al., MIRD pamphlet No. 17: the dosimetry of nonuniform activity distributions–radionuclide S values at the voxel level. Medical Internal Radiation Dose Committee. J Nucl Med, 1999. 40(1): p. 11S-36S.
97. Costes, S.V., L.G. Bouchet, and W.E. Bolch, Cubical S values for use with SPECT, PET, and autoradiographic imaging data in performing small-scale dosimetry. Health Physics, 1996. 70(6 SUPPL.): p. S44-S45.